Abstract
Factors associated with diarrhea in a unit of intensive therapy: Cohort study
Author(s): Rodrigues de Barros, Josiane1; Fraga Lobo, Iza Maria2; Melo Soares, Fabiana1; Ferreira de Almeida, Daniela Santos Silva2
Introduction: Diarrhea is considered one of the most frequent complications in intensive care unit (ICU) patients. The variation of the data on its incidence may be a result of the inconsistency of the definitions adopted. The causes are complex and multifactorial, but several contributing factors are described.
Objectives: To determine the incidence and factors associated with diarrhea in patients admitted to an ICU of a public hospital.
Methods: This is a prospective cohort-type study, whose population was composed of 103 adult patients (≥ 18 years old) using exclusive enteral nutritional therapy hospitalized in a clinical adult ICU at a public emergency hospital. The occurrence of diarrhea was defined as the presence of 3 or more liquid or pasty stools in 24 hours and the possible associated factors were: nutritional therapy, presence of fever, infection, hypoalbuminemia, medications in use. Descriptive statistical analysis and relative risk calculation were performed using the Epi-info® version 7 program. For comparisons between the groups, Student’s t-test and chi-square or Fischer’s exact test were used, where appropriate, with level of statistical significance established at P <0.05.
Results: Out of 103 patients, 46.6% (48) presented diarrhea with a mean duration of 1.3 days (± 2.1). The group with diarrhea had a longer residence time than patients without diarrhea - 37 x 20.3 days (p = 0.002). Risk factors associated with diarrhea were: presence of fever (RR = 1.96), presence of hypoalbuminemia (RR = 1.54), prokinetic use (RR = 1.86), use of carbapenems (RR = 1.71) and glycopeptides (RR = 2.1).
Conclusion: The incidence of diarrhea in patients using nutritional therapy in the unit studied was high, but similar to other data reported in the literature.
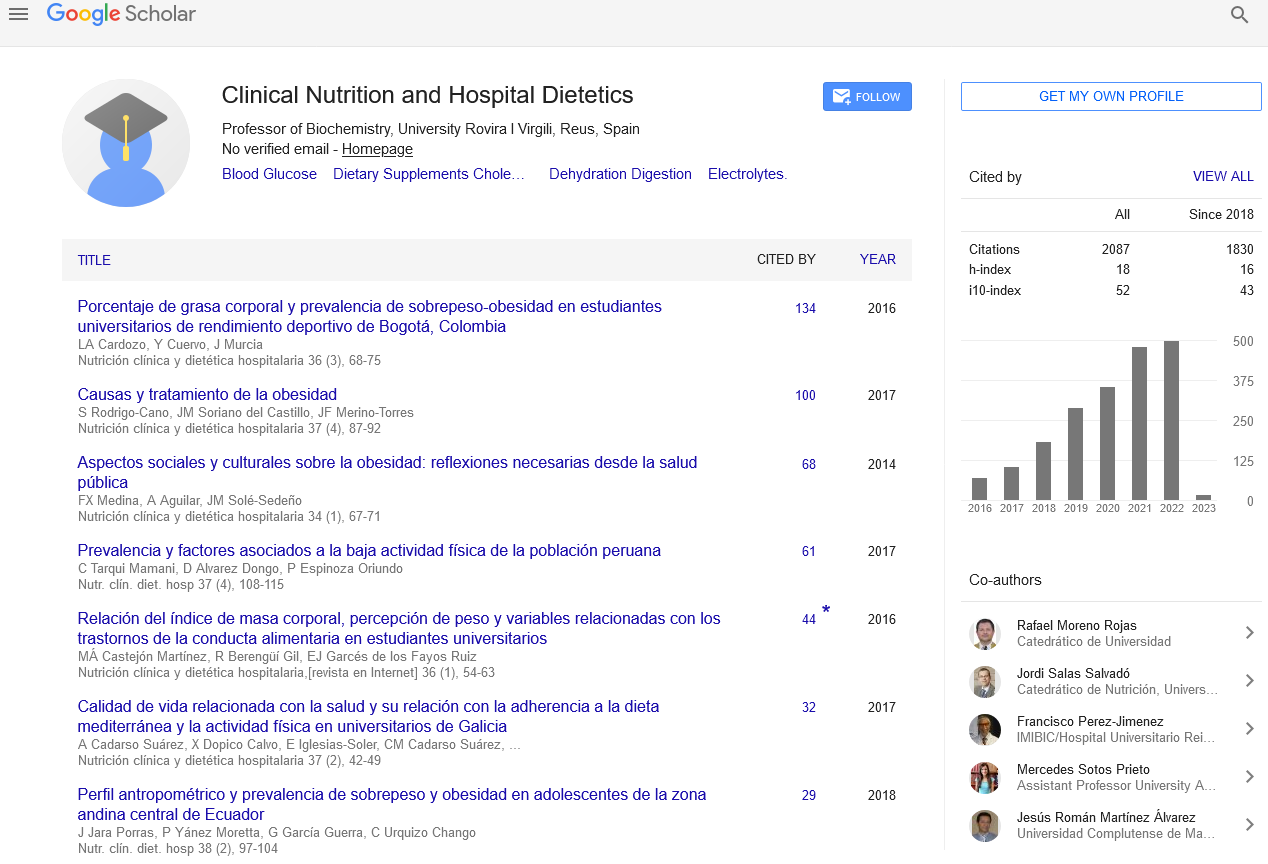
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics