Advanced clinical nutrition: Integrative approaches for hospitalized patients
Opinion Article - (2024) Volume 44, Issue 1
Received: 21-Feb-2024, Manuscript No. CNHD-24-135012; Editor assigned: 23-Feb-2024, Pre QC No. CNHD-24-135012; Reviewed: 08-Mar-2024, QC No. CNHD-24-135012; Revised: 15-Mar-2024, Manuscript No. CNHD-24-135012; Published: 22-Mar-2024, DOI: 10.12873/0211-6057.44.01.217
Description
Advanced clinical nutrition plays a pivotal role in the comprehensive care of hospitalized patients. By integrating various nutritional strategies tailored to individual needs, healthcare providers can significantly enhance patient outcomes, support recovery, and improve overall health. Personalized nutritional assessments and plans are fundamental in delivering effective clinical nutrition to hospitalized patients. These tailored approaches consider the unique metabolic, physiological, and medical conditions of each patient, ensuring optimal nutritional support.
Personalized nutritional assessments and plans
Comprehensive nutritional assessments: Accurate nutritional assessment is the first step in developing a personalized nutritional plan. This involves a thorough evaluation of the patient’s dietary history, biochemical data, clinical status, and anthropometric measurements. Advanced tools like Bioelectrical Impedance Analysis (BIA), Dual-Energy X-Ray Absorptiometry (DEXA), and indirect calorimetry provide detailed insights into body composition, energy expenditure, and nutrient requirements.
Individualized nutritional requirements: Hospitalized patients often have unique nutritional needs due to their underlying medical conditions, treatments, and metabolic stress. For instance, patients with severe burns require significantly higher protein and calorie intake to support wound healing and recovery. Similarly, those with renal failure may need restricted protein and electrolyte intake to prevent further kidney damage. Personalized nutritional plans are designed to meet these specific needs, ensuring adequate and appropriate nutrient delivery.
Dietary modifications: Based on the nutritional assessment, dietary modifications are made to address specific health issues. For example, a patient with cardiovascular disease might benefit from a low-sodium, heart-healthy diet, while a patient with diabetes may require a diet with controlled carbohydrate intake to manage blood sugar levels. These modifications are essential for managing symptoms, preventing complications, and supporting overall health.
Interdisciplinary collaboration: Developing and implementing personalized nutritional plans require close collaboration among dietitians, physicians, nurses, and other healthcare professionals. This interdisciplinary approach ensures that all aspects of the patient’s health are considered and that nutritional interventions are integrated seamlessly into the overall treatment plan.
Integrative nutritional therapies and techniques
Integrative nutritional therapies and techniques encompass a wide range of strategies aimed at optimizing the nutritional status and health outcomes of hospitalized patients. These advanced interventions leverage the latest research and clinical practices to provide comprehensive nutritional care.
Medical Nutrition Therapy (MNT): MNT involves the use of specific nutritional interventions to manage medical conditions. For instance, Enteral Nutrition (EN) is preferred for patients who can tolerate it, as it maintains gut integrity and function. For patients unable to use their gastrointestinal tract, Parenteral Nutrition (PN) provides essential nutrients intravenously. MNT is tailored to each patient’s needs, ensuring they receive the right balance of macronutrients and micronutrients.
Specialized nutritional formulas: Specialized enteral and parenteral formulas are designed to meet the unique needs of specific patient populations. High-protein formulas support muscle preservation and immune function, while low-carbohydrate formulas help manage blood sugar levels in diabetic patients. Immunonutrition formulas, enriched with omega-3 fatty acids, glutamine, and antioxidants, are beneficial for patients undergoing major surgery or those with critical illnesses, as they help modulate the immune response and reduce inflammation.
Micronutrient supplementation: Micronutrient deficiencies are common in hospitalized patients due to their increased metabolic demands and altered nutrient absorption. Supplementing essential vitamins and minerals, such as vitamin D, zinc, and selenium, can support immune function, wound healing, and overall recovery. Tailored supplementation plans are developed based on individual deficiencies identified through laboratory testing.
Probiotics and prebiotics: Gut health is important for overall health, particularly in hospitalized patients who may experience altered gut flora due to antibiotics and other treatments. Probiotics and prebiotics can help restore healthy gut microbiota, improve gastrointestinal function, and enhance immune responses. These supplements are particularly beneficial for patients with gastrointestinal disorders, such as Inflammatory Bowel Disease (IBD) or Irritable Bowel Syndrome (IBS).
Nutritional support for specific conditions: Certain medical conditions require specialized nutritional support. For example, patients with Chronic Obstructive Pulmonary Disease (COPD) may benefit from a high-calorie, highprotein diet to meet their increased energy needs. Cancer patients often require nutritional strategies to combat malnutrition and cachexia, including high-calorie supplements and appetite stimulants. Tailored nutritional support helps manage symptoms and improves the quality of life for these patients.
Monitoring and adjustments: Continuous monitoring of nutritional interventions is essential to ensure their effectiveness and make necessary adjustments. Regular reassessments of the patient’s nutritional status, tolerance to dietary modifications, and metabolic responses guide the ongoing nutritional care plan. This dynamic approach allows healthcare providers to adapt interventions based on the patient’s evolving clinical condition.
Advanced clinical nutrition, through personalized assessments and integrative therapies, is essential in the comprehensive care of hospitalized patients. By addressing individual nutritional needs and leveraging the latest clinical practices, healthcare providers can significantly enhance patient outcomes, support recovery, and improve overall health. As our understanding of nutrition and its impact on health continues to evolve, integrating these advanced approaches into clinical practice will be paramount in advancing patient care and optimizing health outcomes.
Author Info
Sedat KOTANI*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
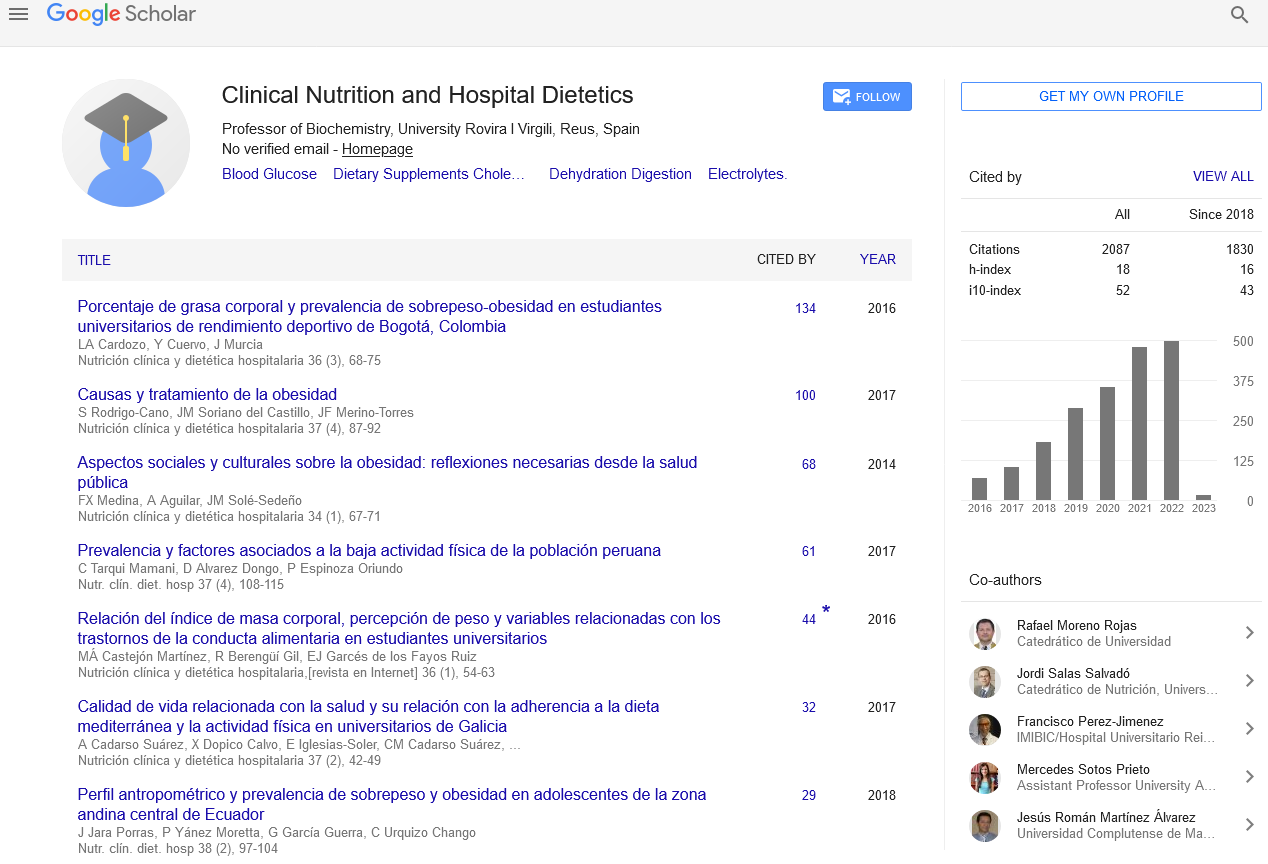
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics