Energy balance in health and disease: Mechanisms and interventions
Short Communication - (2024) Volume 44, Issue 1
Received: 21-Feb-2024, Manuscript No. CNHD-24-135016; Editor assigned: 23-Feb-2024, Pre QC No. CNHD-24-135016; Reviewed: 08-Mar-2024, QC No. CNHD-24-135016; Revised: 15-Mar-2024, Manuscript No. CNHD-24-135016; Published: 22-Mar-2024, DOI: 10.12873/0211-6057.44.01.219
Description
Energy balance is a fundamental concept in understanding human health and disease. It refers to the relationship between energy intake through food and beverages and energy expenditure through basal metabolism, physical activity, and thermogenesis. Maintaining energy balance is crucial for optimal health, while its disruption can lead to various diseases. Understanding the mechanisms that regulate energy balance is essential for addressing both health maintenance and disease prevention. These mechanisms involve a complex interplay between hormonal, neural, and metabolic factors that influence hunger, satiety, and energy expenditure [1,2].
Mechanisms of energy balance
Hormones play a pivotal role in energy balance. Key hormones involved include insulin, leptin, ghrelin, and peptide YY. Insulin, produced by the pancreas, helps regulate blood glucose levels and promotes fat storage. Leptin, secreted by adipose tissue, signals satiety and reduces food intake. Ghrelin, produced in the stomach, stimulates hunger. Peptide YY, released by the gut in response to food intake, promotes satiety. The balance between these hormones helps regulate appetite and energy expenditure [3-5].
The hypothalamus, a region of the brain, is central to energy balance regulation. It integrates signals from hormones and nutrients to control hunger and satiety. The arcuate nucleus within the hypothalamus contains neurons that stimulate appetite (orexigenic) and others that suppress appetite (anorexigenic). The balance of these neural signals influences overall energy intake and expenditure.
Basal Metabolic Rate (BMR), Thermic Effect of Food (TEF), and physical activity are the primary components of energy expenditure. BMR accounts for the majority of daily energy expenditure, representing the energy required for basic physiological functions at rest. TEF refers to the energy required for digestion, absorption, and metabolism of nutrients. Physical activity includes both voluntary exercise and Non-Exercise Activity Thermogenesis (NEAT), such as fidgeting and daily activities [6,7].
Genetic factors significantly contribute to individual differences in energy balance. Genes can affect metabolism, appetite regulation, and fat storage. For example, variations in the FTO gene are associated with increased risk of obesity. Understanding genetic predispositions can help tailor interventions to individual needs [8].
Interventions for managing energy imbalance
Addressing energy imbalances requires a multifaceted approach that includes dietary modifications, physical activity, behavioral strategies, and medical interventions. These interventions aim to restore balance and prevent or treat related diseases such as obesity, diabetes, and cardiovascular diseases.
Reducing caloric intake through portion control and choosing nutrient-dense, low-calorie foods helps create a calorie deficit for weight loss. Balancing macronutrients (carbohydrates, proteins, fats) can influence satiety and metabolism. High-protein diets, for example, can promote satiety and preserve lean muscle mass during weight loss. Meal timing and frequency can impact energy balance. Strategies such as intermittent fasting and eating smaller, frequent meals have shown potential benefits for weight management [9].
Activities such as walking, running, and cycling increase cardiovascular fitness and calorie burning. Strength training exercises help build muscle mass, which increases BMR and promotes fat loss. Incorporating more movement into daily routines, such as taking stairs instead of elevators and engaging in active hobbies, boosts overall energy expenditure.
Paying attention to hunger and satiety cues, eating slowly, and avoiding distractions during meals can prevent overeating. Cognitive-Behavioral Therapy (CBT) and other psychological interventions can help individuals change unhealthy eating patterns and develop healthier habits. Setting realistic, achievable goals for diet and physical activity helps maintain motivation and track progress [10].
Medications such as appetite suppressants and metabolic boosters can aid in weight management for individuals with obesity. Surgical options like gastric bypass and sleeve gastrectomy can be effective for individuals with severe obesity who have not responded to other interventions. These procedures reduce stomach size and alter gut hormones, promoting weight loss. Hormonal therapies may be used to address imbalances in hormones like insulin and leptin, particularly in conditions like diabetes and metabolic syndrome.
Energy balance is a critical aspect of health that involves a complex interplay of hormonal, neural, metabolic, and genetic factors. Understanding these mechanisms provides the foundation for effective interventions to manage energy imbalances. Dietary modifications, increased physical activity, behavioral strategies, and medical interventions all play roles in achieving and maintaining energy balance. By addressing energy imbalances, individuals can prevent and manage diseases such as obesity, diabetes, and cardiovascular disease, ultimately promoting better health and well-being.
Conclusion
- James PT, Rigby N, Leach R. The obesity epidemic, metabolic syndrome and future prevention strategies. Eur J Cardiovasc Prev Rehabil. 2004;11(1):3-8.Crossref]
[Google Scholar] [Pubmed]
- Fernandez L. The metabolic syndrome. Nutr Rev. 2007;65(2):30-34.
[Crossref] [Google Scholar] [Pubmed]
- Stein CJ, Colditz GA. The epidemic of obesity. Journal Clin Endocrinol Metabo. 2004;89(6):2522-2525.
[Crossref] [Google Scholar] [Pubmed]
- Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hyperten Rep. 2018;20(2):1-8.
[Crossref] [Google Scholar] [Pubmed]
- Wahba IM, Mak RH. Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol. 2007;2(3):550-562.
[Crossref] [Google Scholar] [Pubmed]
- Haffner S, Taegtmeyer H. Epidemic obesity and the metabolic syndrome. Circulation. 2003;108:1541-1545.
[Crossref] [Google Scholar] [Pubmed]
- Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. science. 2005;307(5717):1915-1920.
[Crossref] [Google Scholar] [Pubmed]
- Dinan TG, Cryan JF. Brain gut microbiota axis mood, metabolism and behaviour. Nat Rev Gastroenterol Hepatol. 2017;14(2):69-70.
[Crossref] [Google Scholar] [Pubmed]
- Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006; 444(7122):1027-1031.
[Crossref] [Google Scholar] [Pubmed]
- Nehra V, Allen JM, Mailing LJ, Kashyap PC, Woods JA. Gut microbiota: modulation of host physiology in obesity. Physiol. 2016;31(5):327-335.
Author Info
Yara BECHARD*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
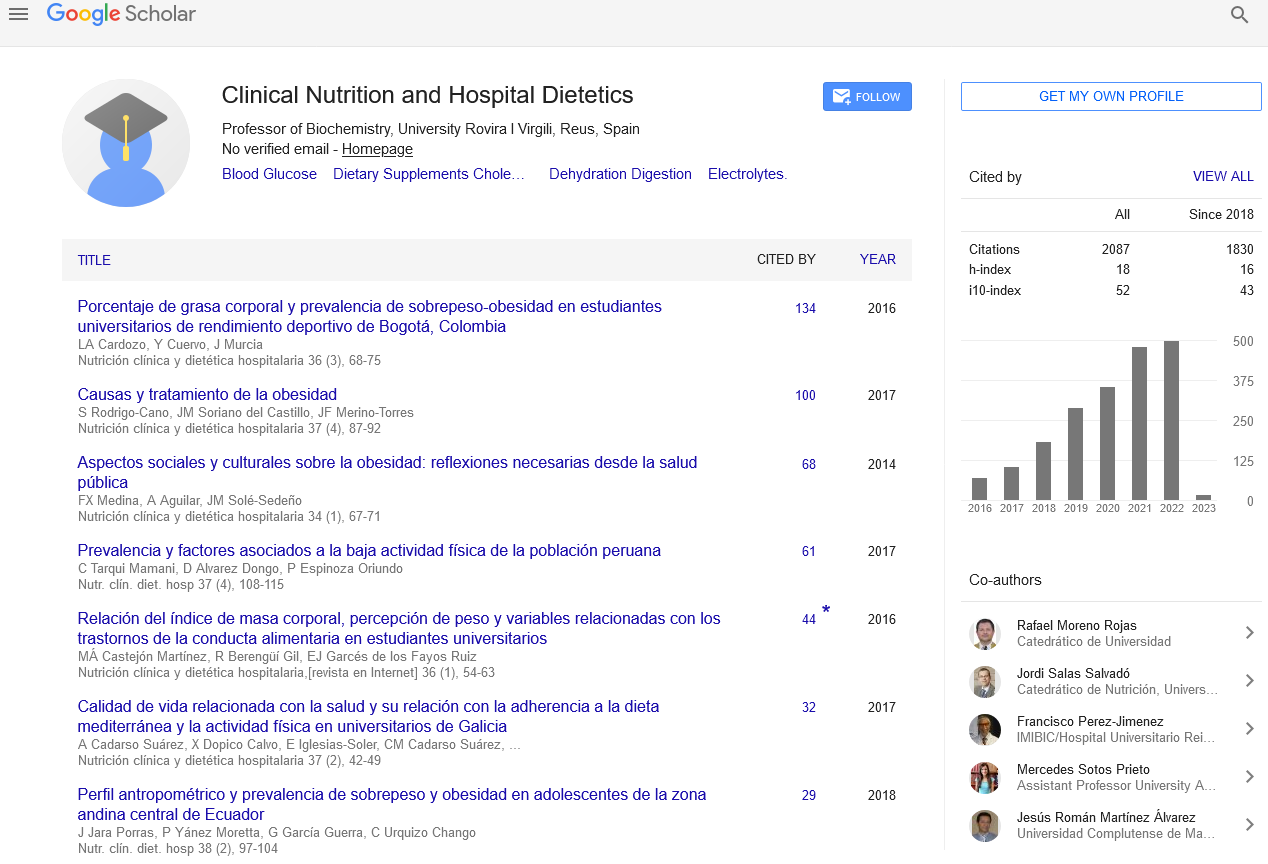
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics