Geriatric nutrition system for health and well-being
Perspective - (2023) Volume 43, Issue 4
Received: 21-Nov-2023, Manuscript No. CNHD-23-123735; Editor assigned: 23-Nov-2023, Pre QC No. CNHD-23-123735 (PQ); Reviewed: 07-Dec-2023, QC No. CNHD-23-123735; Revised: 14-Dec-2023, Manuscript No. CNHD-23-123735 (R); Published: 21-Dec-2023, DOI: 10.12873/0211-6057.43.04.211
Description
The importance of geriatric nutrition becomes increasingly evident. Older adults face unique challenges related to nutritional needs, health conditions, and lifestyle changes. Geriatric nutrition is a specialized field that addresses the dietary requirements of seniors, aiming to optimize their health, prevent illness, and enhance overall well-being. The key considerations of geriatric nutrition, exploring the factors that influence dietary requirements, common nutritional challenges faced by older adults, and the strategies to promote optimal health in the aging population.
Factors influencing geriatric nutrition
Geriatric nutrition is shaped by a combination of physiological, psychological, and social factors. Aging is associated with changes in body composition, metabolism, and nutrient absorption, making it essential to adapt dietary patterns to meet the evolving needs of older adults.
Metabolic changes: Aging often leads to a decrease in basal metabolic rate, meaning that older adults may require fewer calories to maintain their weight. However, the need for certain nutrients, such as protein, calcium, and vitamin D, may increase to support bone health and muscle mass.
Nutrient absorption: The efficiency of nutrient absorption tends to decline with age, impacting the body’s ability to absorb essential vitamins and minerals. As a result, older adults may be at a higher risk of nutrient deficiencies, emphasizing the importance of nutrient-dense food choices.
Hydration: Dehydration is a common concern among older adults due to a diminished sense of thirst and changes in kidney function. Ensuring proper hydration is crucial for maintaining cognitive function, preventing constipation, and supporting overall health.
Chronic health conditions: The prevalence of chronic health conditions, such as diabetes, cardiovascular disease, and osteoporosis, increases with age. Geriatric nutrition must address these conditions through dietary modifications that manage symptoms and promote better health outcomes.
Nutritional challenges in geriatric nutrition
Several challenges contribute to the complexity of geriatric nutrition, requiring a tailored approach to address the unique needs of older adults.
Malnutrition: Malnutrition is a significant concern in the geriatric population, often resulting from factors such as reduced appetite, impaired nutrient absorption, and chronic illnesses. It can contribute to muscle wasting, fatigue, and compromised immune function.
Dental health: Poor oral health can impact the ability to chew and swallow, affecting dietary choices and nutrient intake. Dental problems may lead to a preference for softer, easily chewable foods, potentially limiting the variety of nutrients consumed.
Medication interactions: Older adults often take multiple medications, and some may interact with nutrients or affect appetite. Understanding these interactions is crucial in managing nutrition for seniors effectively.
Social isolation: Loneliness and social isolation can negatively impact dietary habits. Older adults who live alone may be less motivated to prepare balanced meals, leading to potential nutritional deficiencies.
Strategies for promoting optimal geriatric nutrition
Balanced diet: Emphasizing a balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and dairy or dairy alternatives is fundamental. Adequate intake of vitamins and minerals supports overall health and reduces the risk of chronic diseases.
Protein intake: Protein is crucial for maintaining muscle mass, bone health, and immune function. Including protein- rich foods such as lean meats, poultry, fish, eggs, dairy, and plant-based sources in the diet is essential for older adults.
Hydration awareness: Encouraging regular fluid intake, including water and hydrating foods like fruits and vegetables, is vital to prevent dehydration. Monitoring urine color and paying attention to signs of thirst can help older adults stay adequately hydrated.
Regular physical activity: Engaging in regular physical activity supports overall health, muscle strength, and bone density. Combined with proper nutrition, exercise contributes to maintaining functional independence and reducing the risk of falls.
Regular health check-ups: Routine health check-ups help identify and address nutritional deficiencies or health conditions promptly. Regular monitoring ensures that dietary recommendations align with changing health needs.
Social support: Combatting social isolation is crucial for promoting healthy eating habits. Encouraging social interactions, community engagement, and shared meals can positively impact nutritional well-being.
Geriatric nutrition plays a pivotal role in supporting the health and vitality of older adults. Understanding the unique challenges and factors influencing nutritional needs in the aging population is essential for healthcare professionals, caregivers, and older individuals themselves. By implementing tailored dietary strategies, promoting hydration, and addressing the multifaceted aspects of geriatric nutrition, we can enhance the quality of life for seniors and support healthy aging.
Author Info
Alfehaidi CARRIQUIRY*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
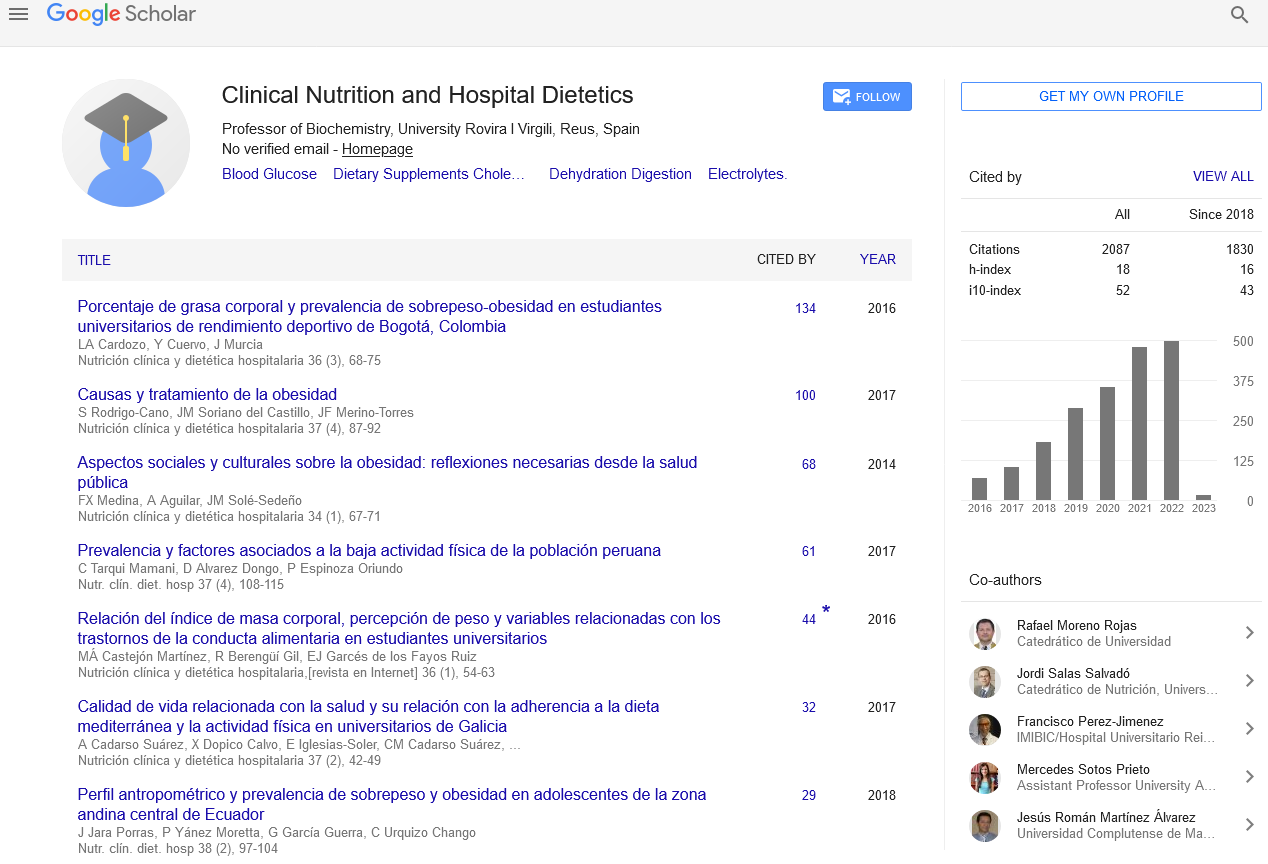
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics