Optimizing nutritional interventions in critical care environments
Perspective - (2024) Volume 44, Issue 1
Received: 21-Feb-2024, Manuscript No. CNHD-24-135008; Editor assigned: 23-Feb-2024, Pre QC No. CNHD-24-135008; Reviewed: 08-Mar-2024, QC No. CNHD-24-135008; Revised: 15-Mar-2024, Manuscript No. CNHD-24-135008; Published: 22-Mar-2024, DOI: 10.12873/0211-6057.44.01.216
Description
In critical care Environments, nutritional interventions are a cornerstone of patient management, profoundly influencing recovery outcomes and overall health. The unique physiological stresses faced by critically ill patients necessitate meticulously tailored nutritional strategies. Critically ill patients present unique challenges in nutritional assessment and delivery due to their altered metabolic states and the impact of various medical interventions. Effective nutritional strategies must address these complexities to support recovery and improve outcomes.
Challenges and strategies in nutritional assessment and delivery
Metabolic alterations and nutritional requirements: Critically ill patients often experience hypermetabolism, catabolism, and inflammatory responses, which can significantly increase their nutritional requirements. Accurate assessment of energy needs is crucial and can be achieved through indirect calorimetry or predictive equations adjusted for stress factors. Ensuring an adequate intake of macronutrients (proteins, fats, and carbohydrates) and micronutrients (vitamins and minerals) is essential to meet these heightened demands.
Assessing nutritional status: Traditional methods of nutritional assessment, such as weight and Body Mass Index (BMI), may be unreliable in critical care due to fluid imbalances and edema. Instead, biochemical markers (e.g., serum albumin, prealbumin), anthropometric measurements, and clinical history are utilized to gauge nutritional status. Advanced tools like Bioelectrical Impedance Analysis (BIA) and Dual-Energy X-Ray Absorptiometry (DEXA) can also provide more accurate assessments of body composition.
Delivery methods: Enteral Nutrition (EN) is preferred over Parenteral Nutrition (PN) due to its lower risk of infections and complications, as well as its positive effects on gut integrity and immune function. However, EN may not always be feasible due to gastrointestinal dysfunctions. In such cases, PN becomes necessary, but must be carefully managed to avoid complications like hyperglycemia, liver dysfunction, and infections. A combined approach, initiating EN as early as possible while supplementing with PN if required, can be beneficial.
Timing and initiation of nutrition: Early nutritional intervention, ideally within 24-48 hours of ICU admission, is associated with better outcomes. Early EN helps maintain gut integrity, modulate immune responses, and reduce the risk of sepsis. Gradual initiation and careful monitoring of tolerance are crucial to prevent complications like refeeding syndrome.
Evidence-based nutritional protocols for critical care
Implementing evidence-based nutritional protocols in critical care settings ensures standardized, highquality nutritional support tailored to the specific needs of critically ill patients. These protocols encompass guidelines on macronutrient distribution, micronutrient supplementation, and specific nutritional strategies for various conditions.
Protein requirements: Adequate protein intake is vital for preserving lean body mass and supporting immune function. Critically ill patients often require higher protein intake, typically ranging from 1.2 to 2.0 grams per kilogram of body weight per day. Specific conditions, such as burns or trauma, may necessitate even higher protein requirements. The use of high-protein enteral formulas can help meet these needs effectively.
Micronutrient supplementation: Critically ill patients are at risk of deficiencies in essential vitamins and minerals, including vitamins A, C, D, E, and zinc, selenium, and magnesium. Supplementation of these micronutrients, tailored to individual deficiencies, can support immune function, wound healing, and overall recovery. Regular monitoring of micronutrient levels is necessary to guide supplementation.
Specialized nutritional formulas: In specific conditions, such as Acute Respiratory Distress Syndrome (ARDS) or sepsis, specialized nutritional formulas enriched with omega-3 fatty acids, antioxidants, and immunomodulatory nutrients can provide additional benefits. These formulas can help modulate inflammatory responses, improve oxygenation, and enhance clinical outcomes.
Glycemic control: Maintaining optimal glycemic control is critical in critically ill patients to prevent hyperglycemiarelated complications. Nutritional strategies, including the use of low-glycemic index formulas and continuous insulin infusions, can help achieve target blood glucose levels. Regular monitoring and adjustments are essential to balance the risks of hyperglycemia and hypoglycemia.
Monitoring and adjustments: Continuous monitoring of nutritional interventions is essential to ensure their efficacy and adjust for changes in clinical status. This involves regular assessment of nutritional intake, tolerance, and metabolic responses, as well as adjustments based on evolving clinical conditions. Multidisciplinary collaboration among dietitians, physicians, nurses, and pharmacists is crucial for optimizing nutritional care.
Optimizing nutritional interventions in critical care settings is a multifaceted process that requires careful assessment, evidence-based protocols, and continuous monitoring. By addressing the unique metabolic needs of critically ill patients and employing tailored nutritional strategies, healthcare providers can significantly enhance patient outcomes, support recovery, and reduce complications. As the understanding of clinical nutrition continues to evolve, integrating these insights into practice will be paramount in advancing critical care and improving patient survival and quality of life.
Author Info
Micaela BERNARDES*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
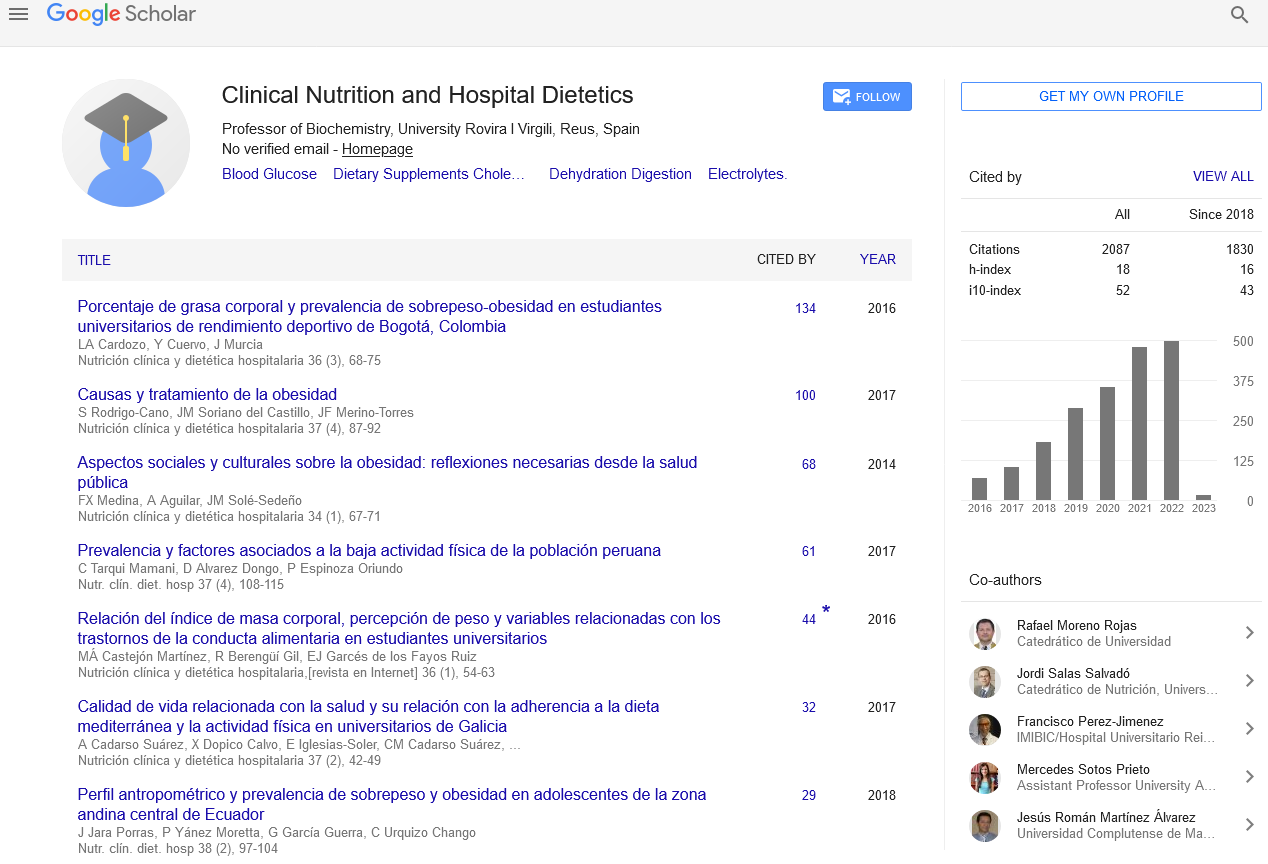
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics