Personalized nutrition for gastrointestinal health
Opinion Article - (2024) Volume 44, Issue 2
Received: 22-May-2024, Manuscript No. CNHD-24-143694; Editor assigned: 24-May-2024, Pre QC No. CNHD-24-143694 (PQ); Reviewed: 07-Jun-2024, QC No. CNHD-24-143694; Revised: 14-Jun-2024, Manuscript No. CNHD-24-143694 (R); Published: 21-Jun-2024, DOI: 10.12873/0211-6057.44.02.224
Description
Gastrointestinal (GI) disorders encompass a wide range of conditions that affect the digestive tract, including Inflammatory Bowel Disease (IBD), Irritable Bowel Syndrome (IBS), celiac disease, and Gastroesophageal Reflux Disease (GERD). Nutritional interventions have gained prominence as an important aspect of managing these disorders due to their potential to alleviate symptoms, improve quality of life, and support overall health. By tailoring dietary strategies to individual needs, patients can experience significant benefits in symptom management and disease progression.
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease, including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. Nutritional interventions can play a key role in managing IBD by addressing malnutrition, reducing inflammation, and supporting gut healing. The low-FODMAP diet has been shown to help reduce symptoms in patients with IBD. FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are short-chain carbohydrates that can ferment in the gut and exacerbate symptoms. Reducing the intake of high-FODMAP foods can help minimize bloating, gas, and abdominal pain.
The SCD focuses on eliminating complex carbohydrates that may contribute to gut inflammation. By restricting grains, legumes, and certain sugars, the diet aims to reduce symptoms and promote gut health. Although more research is needed, some patients report improvement with this approach. Incorporating anti- inflammatory foods, such as omega-3 fatty acids found in fish and flaxseeds, as well as antioxidants from fruits and vegetables, can help manage inflammation. A diet rich in these nutrients may support overall gut health and reduce flare-ups.
Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome is a functional GI disorder characterized by symptoms such as abdominal pain, bloating, and changes in bowel habits. Nutritional interventions can help manage these symptoms and improve quality of life. Similar to IBD, the low-FODMAP diet is effective for many patients with IBS. By eliminating high-FODMAP foods, individuals can experience reduced symptoms of bloating, gas, and diarrhea. Reintroducing FODMAPs in a controlled manner helps identify specific triggers. Incorporating soluble fiber sources, such as oats, psyllium, and apples, can help manage IBS symptoms, especially in those with constipation-predominant IBS. Soluble fiber helps to regulate bowel movements and improve stool consistency.
Probiotics, which are beneficial bacteria found in fermented foods or supplements, may help balance gut microbiota and improve IBS symptoms. While more research is needed to determine the most effective strains and dosages, some patients find relief with probiotic use.
Celiac disease
Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. Strict adherence to a gluten-free diet is essential for managing celiac disease and preventing damage to the small intestine. The cornerstone of managing celiac disease is a lifelong gluten-free diet. This involves avoiding all sources of gluten, including wheat, barley, rye, and their derivatives. Patients must also be vigilant about cross-contamination in foods and beverages. Individuals with celiac disease may experience deficiencies in essential nutrients, such as iron, calcium, and vitamin D, due to malabsorption. Supplementing these nutrients can help address deficiencies and support overall health. Regular monitoring and consultation with a healthcare provider are essential to tailor supplementation needs.
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease is a chronic condition where stomach acid frequently flows back into the esophagus, causing symptoms such as heartburn and regurgitation. Nutritional interventions can help reduce symptoms and manage GERD effectively. Avoiding high-acidity foods and beverages, such as citrus fruits, tomatoes, and coffee, can help reduce acid reflux symptoms. Opting for low-acidity alternatives and eating smaller, more frequent meals can also alleviate discomfort. A diet high in fiber can help manage GERD symptoms by promoting digestion and reducing the likelihood of acid reflux. Foods such as whole grains, fruits, and vegetables can aid in digestion and support overall gastrointestinal health. Identifying and avoiding personal trigger foods, such as spicy dishes, fatty foods, and chocolate, can help minimize GERD symptoms. Keeping a food diary can assist in pinpointing specific triggers and making necessary dietary adjustments.
The role of personalized nutrition in gastrointestinal health
Personalized nutrition involves tailoring dietary recommendations to an individual’s unique needs, taking into account their specific gastrointestinal condition, genetic factors, and lifestyle. This approach can enhance the effectiveness of nutritional interventions and support better management of GI disorders. Genetic testing can provide insights into an individual’s predisposition to certain gastrointestinal conditions and their potential responses to different dietary interventions. This information can guide personalized dietary strategies and improve overall outcomes. In addition to dietary changes, considering lifestyle factors such as stress management, physical activity, and sleep can further support gastrointestinal health. Integrating these elements into a comprehensive management plan can optimize symptom control and improve quality of life.
Nutritional interventions are a critical component of managing gastrointestinal disorders, offering tailored strategies to address symptoms, improve gut health, and enhance overall well-being. By adopting personalized nutrition plans based on individual needs and conditions, patients can experience significant benefits and achieve better outcomes in managing their gastrointestinal health. As research in this field continues to evolve, the integration of nutritional strategies into comprehensive treatment plans will play an increasingly important role in improving the lives of those affected by GI disorders.Author Info
Bauer SOUBEYRAN*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
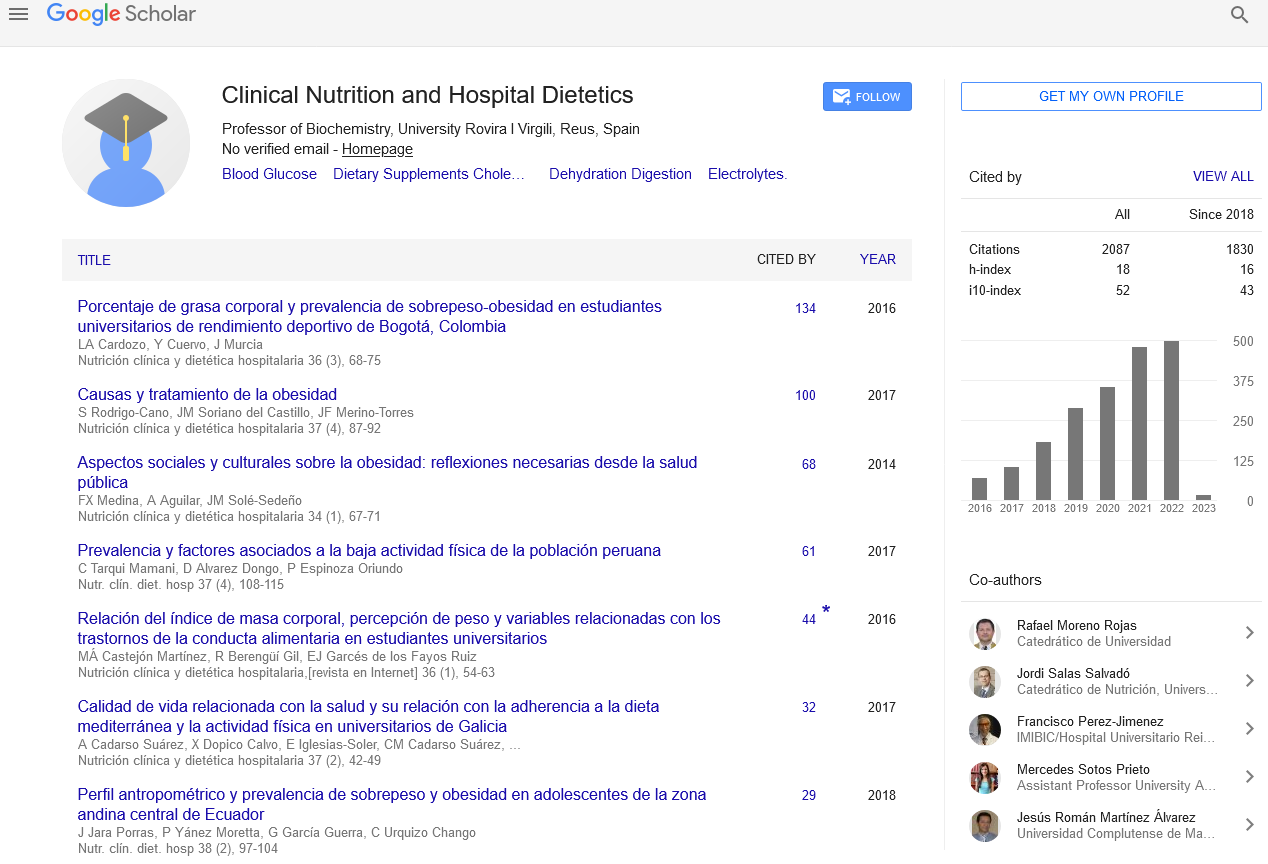
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics