The impact of enteral nutrition on gastrointestinal recovery in surgical patients
Perspective - (2024) Volume 44, Issue 3
Received: 21-Aug-2024, Manuscript No. CNHD-24-151894; Editor assigned: 23-Aug-2024, Pre QC No. CNHD-23-151894 (PQ); Reviewed: 06-Sep-2024, QC No. CNHD-23-151894; Revised: 13-Sep-2024, Manuscript No. CNHD-23-151894 (R); Published: 20-Sep-2024, DOI: 10.12873/0211-6057.44.03.226
Description
Enteral Nutrition (EN) involves delivering nutrients directly into the Gastrointestinal (GI) tract through a feeding tube, commonly used when patients are unable to eat or absorb nutrients orally. In surgical patients, particularly those undergoing gastrointestinal surgery, EN plays a vital role in supporting nutritional needs, promoting gastrointestinal recovery and enhancing overall recovery.
Role of enteral nutrition in GI recovery
The gut plays an essential role in the body’s immune function and nutrient absorption. After surgery, especially abdominal or gastrointestinal surgeries, the gut is often temporarily impaired due to anesthesia, trauma and surgical stress. Enteral nutrition helps preserve gut function by providing continuous nutrients, preventing gut atrophy and maintaining mucosal integrity. It supports the GI system’s natural healing processes by stimulating the gut, which helps prevent complications like infections and gut permeability, which can lead to systemic inflammatory responses or sepsis.
Post-surgery patients have increased metabolic needs and adequate nutrition is different for tissue repair, immune function and overall recovery. Enteral nutrition provides a reliable source of essential macronutrients (proteins, fats and carbohydrates) and micronutrients (vitamins and minerals) that aid in the recovery process. Unlike parenteral nutrition, which bypasses the GI tract entirely, EN directly stimulates the digestive system and provides a more natural route for nutrient absorption.
This stimulation supports digestion, promotes gut motility and helps reduce the risk of malnutrition.
One of the significant concerns post-surgery is delayed gastric emptying and reduced gut motility, often resulting in ileus (a condition of slowed or absent intestinal movement). Enteral feeding can help promote the return of gastrointestinal motility. Even when full motility is not restored immediately, EN stimulates the gut’s muscular contractions and encourages peristalsis. This not only facilitates quicker resumption of normal bowel function but also helps reduce the duration of ileus and contributes to a faster recovery.
Surgical patients are at a higher risk for infections and complications due to the stress of surgery and the potential for weakened immune function. EN has been shown to reduce the incidence of infections such as pneumonia, surgical site infections and sepsis. By maintaining gut function and integrity, enteral nutrition supports the immune system and helps in wound healing. Moreover, EN positively affects the gut microbiota, reducing the chances of harmful bacteria overgrowth that could lead to infections.
Clinical and economic benefits
Enteral nutrition not only improves clinical outcomes by speeding up recovery but also has significant economic benefits. Early initiation of EN has been associated with shorter hospital stays, reduced use of parenteral nutrition and fewer complications, ultimately lowering healthcare costs. A quicker recovery and reduced infection rates allow patients to leave the hospital sooner, reducing both direct medical costs and indirect costs related to extended hospitalizations.
Some patients may struggle with tolerating enteral nutrition, especially those with significant gastric or intestinal dysfunction. Complications such as nausea, vomiting and diarrhea can arise, which may hinder the positive effects of EN. In some cases, feeding intolerance or aspiration can lead to additional complications, so proper monitoring is essential. The timing of EN initiation remains a subject of debate. While early enteral feeding, ideally within 24 hours to 48 hours post-surgery, is associated with better outcomes, some patients may not be stable enough to tolerate feeding that early. For those who are unstable or who have severe GI issues, delaying enteral feeding until the patient’s condition improves may be necessary. Each case should be assessed individually to determine the optimal time to begin EN. Enteral nutrition formulas must be tailored to the patient’s individual needs. Surgical patients may require specialized formulas based on their condition, such as those with specific dietary needs due to diabetes, kidney issues, or liver dysfunction. Choosing the correct formula ensures that patients receive adequate nutrition without overloading the digestive system.
Enteral nutrition is a key component of postoperative care, providing essential support to the gastrointestinal system during recovery. By maintaining gut integrity, enhancing nutritional status, promoting motility and reducing infection risks, EN plays a different role in improving the outcomes for surgical patients. Although challenges related to tolerability, timing and formulation exist, the benefits of enteral nutrition in facilitating gastrointestinal recovery and reducing hospital stays make it an indispensable tool in modern surgical care. With careful management, EN can significantly enhance recovery and contribute to the overall well-being of surgical patients.
Author Info
Connie LACHAT*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
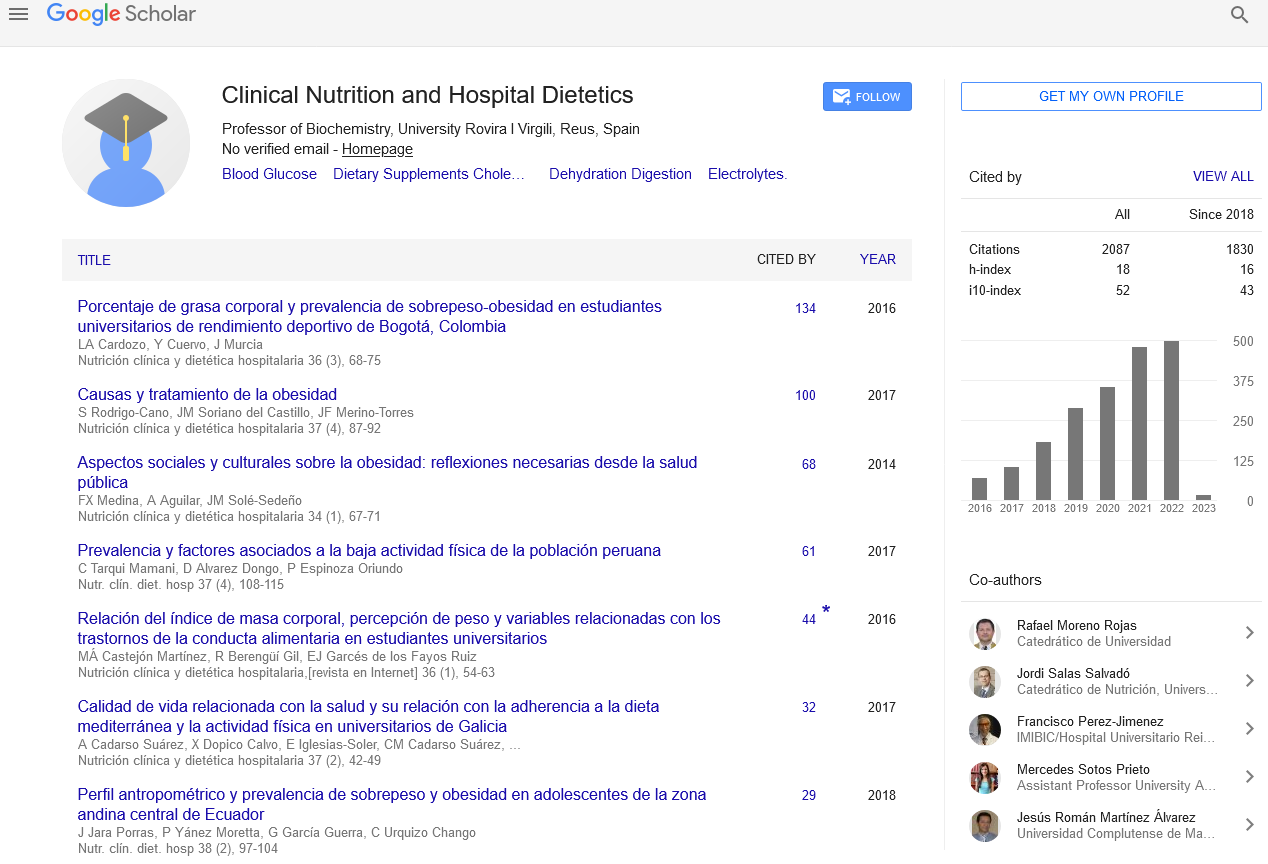
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics