The impact of metabolic syndrome on mental health
Perspective - (2024) Volume 44, Issue 3
Received: 21-Aug-2024, Manuscript No. CNHD-24-151896; Editor assigned: 23-Aug-2024, Pre QC No. CNHD-23-151896 (PQ); Reviewed: 06-Sep-2024, QC No. CNHD-24-151896; Revised: 13-Sep-2024, Manuscript No. CNHD-23-151896 (R); Published: 20-Sep-2024, DOI: 10.12873/0211-6057.44.03.227
Description
Metabolic syndrome is a collection of conditions that increase the risk of developing heart disease, stroke and type 2 diabetes. It is characterized by a combination of factors, including high blood pressure, high blood sugar, excess abdominal fat and abnormal cholesterol levels. As the prevalence of metabolic syndrome continues to rise globally, there is increasing evidence suggesting that it not only affects physical health but also has a significant impact on mental health. The relationship between metabolic syndrome and mental health disorders, such as depression, anxiety and cognitive decline, has become an area of growing concern.
Physiological link between metabolic syndrome and mental health
Metabolic syndrome influences mental health through several physiological mechanisms. The chronic inflammation associated with metabolic syndrome is a key factor contributing to mental health disturbances. Inflammation has been implicated in the pathogenesis of both physical diseases, such as cardiovascular disease and psychiatric conditions like depression and anxiety. Studies show that the presence of increased inflammatory markers, such as C-Reactive Protein (CRP), is higher in individuals with metabolic syndrome and these elevated levels are also linked to depression and anxiety symptoms.
Additionally, metabolic syndrome is often accompanied by insulin resistance, which can directly affect brain function. Insulin plays an important role in regulating brain metabolism and its resistance can lead to impaired neurotransmitter function and increased oxidative stress, both of which are associated with cognitive decline and mood disorders. The connection between insulin resistance and mental health is particularly evident in conditions like depression, where disrupted glucose metabolism in the brain may exacerbate mood symptoms.
Moreover, the presence of visceral fat, which is a characteristic of metabolic syndrome, can also affect the brain. Excess fat tissue can release pro-inflammatory cytokines and other substances that disrupt the normal function of the brain’s neural circuits, leading to mood disorders and cognitive deficits. As a result, individuals with metabolic syndrome are at an increased risk of developing depression, anxiety and other mood disorders, which can, in turn, increase the severity of the syndrome itself.
Mental health implications and strategies for intervention
The impact of metabolic syndrome on mental health is a two-way street, where each condition can influence the progression of the other. For instance, the presence of mental health disorders, such as depression and anxiety, can increase the likelihood of developing metabolic syndrome. People experiencing chronic stress, for example, may engage in unhealthy coping mechanisms, such as poor diet, lack of physical activity and smoking, which contribute to the risk factors for metabolic syndrome. Additionally, stress-related changes in the Hypothalamic-Pituitary-Adrenal (HPA) axis, which regulates the body’s stress response, can contribute to insulin resistance, elevated blood pressure and other components of metabolic syndrome.
Conversely, the presence of metabolic syndrome can also worsen mental health outcomes. The physical discomfort and limitations caused by metabolic syndrome symptoms such as fatigue, weight gain and increased risk of cardiovascular events can lead to a sense of helplessness, low self-esteem and depression. Chronic health conditions associated with metabolic syndrome can create a vicious cycle where worsening physical health fuels mental health issues and mental health problems make it harder to manage the physical aspects of metabolic syndrome.
The good news is that early intervention in managing metabolic syndrome can positively impact both physical and mental health. Adopting a healthy lifestyle, including regular physical activity, a balanced diet and stress management techniques, can significantly reduce the severity of metabolic syndrome and improve mental health outcomes. Physical activity, for instance, has been shown to reduce inflammation, improve insulin sensitivity and enhance brain function, all of which are beneficial for both managing metabolic syndrome and improving mood. Cognitive-Behavioral Therapy (CBT) and other forms of psychotherapy can also be useful for patients with both metabolic syndrome and mental health concerns, as they help address stress, depression and anxiety, promoting healthier coping strategies and lifestyle changes.
Additionally, pharmacological treatments targeting both metabolic and mental health issues can be considered. For example, medications like antidepressants may be prescribed to manage depression or anxiety, while medications to control blood pressure, cholesterol and blood sugar can help manage metabolic syndrome. However, a comprehensive approach that addresses both the physical and mental health components of metabolic syndrome is important for achieving the best outcomes.
The relationship between metabolic syndrome and mental health is complex and bidirectional, with each condition influencing the other. Metabolic syndrome contributes to mental health issues through physiological mechanisms such as inflammation, insulin resistance and altered fat metabolism. Meanwhile, mental health problems like depression and anxiety can worsen the progression of metabolic syndrome by promoting unhealthy behaviors and stress-related physiological changes. Understanding this connection is essential for developing comprehensive treatment strategies that address both the physical and mental aspects of health. By promoting lifestyle changes, managing stress and considering both pharmacological and psychological interventions, healthcare providers can help individuals with metabolic syndrome improve both their physical and mental well-being.
Author Info
Finkelstein KRAISID*Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
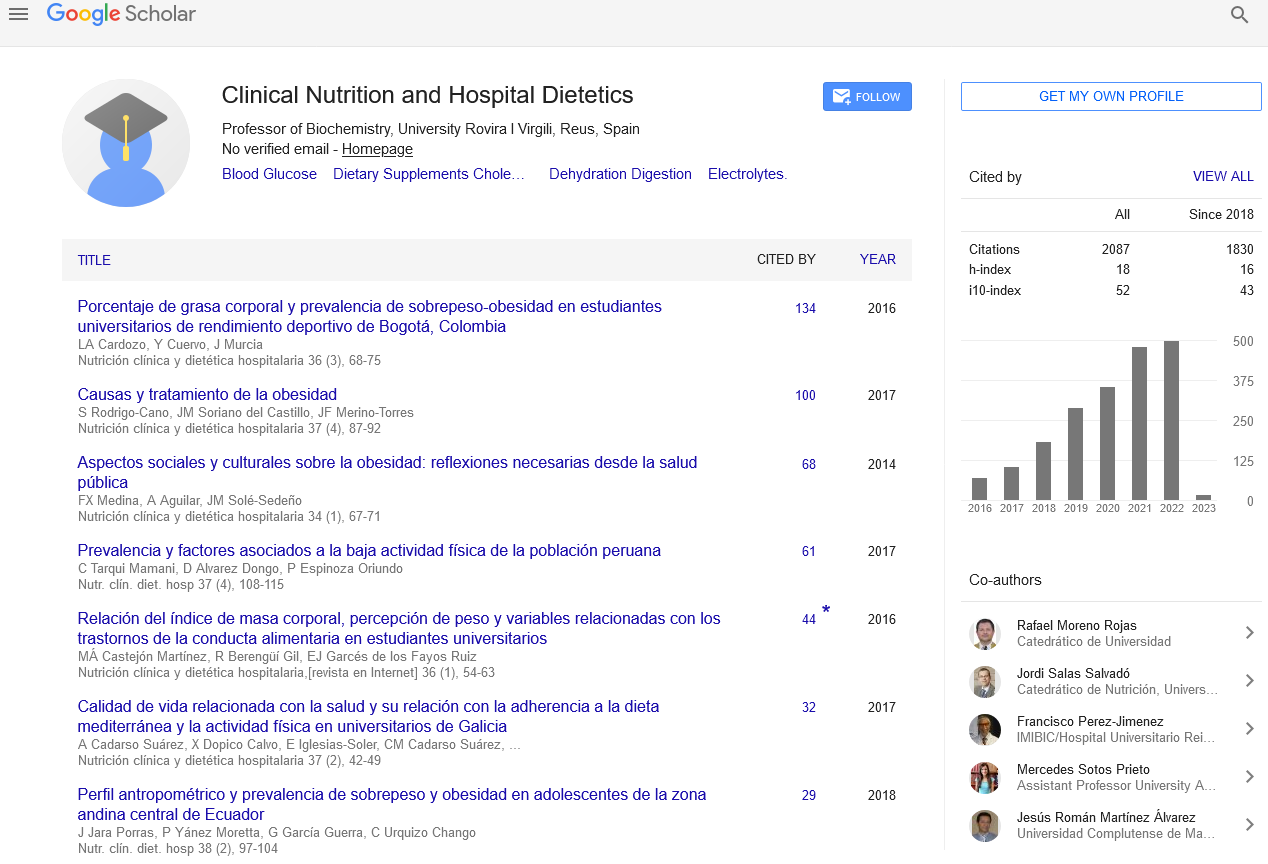
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics