Trends in fruit and vegetables consumption among Malaysian adults, 2006-2019
Research - (2023) Volume 43, Issue 4
Received: 15-Nov-2023, Manuscript No. CNHD-23-120155; Editor assigned: 17-Nov-2023, Pre QC No. CNHD-23-120155 (PQ); Reviewed: 01-Dec-2023, QC No. CNHD-23-120155; Revised: 08-Dec-2023, Manuscript No. CNHD-23-120155 (R); Published: 15-Dec-2023, DOI: 10.12873/0211-6057.43.04.205
Abstract
Introduction: Inadequate fruit and vegetables consumption is linked to cardiovascular diseases, type 2 diabetes, and certain types of cancers, obesity and all-cause mortality. Although the Malaysian Dietary Guidelines 2020 recommended the consumption of at least two servings of fruit and three servings of vegetables daily in the adults, data from several National Health and Morbidity Survey among the Malaysian adults showed remarkedly low prevalence of adequate fruit and vegetables consumption.
Objective: We aimed to determine the trend in fruit and vegetables consumption among the Malaysian adults between 2006 and 2019.
Methodology: We analysed data from five nationally representative, cross-sectional national surveys, namely the Malaysian Non-Communicable Disease Surveillance 2006 (MyNCDS-1), the National Health and Morbidity Survey (NHMS) 2011, the NHMS 2014, NHMS 2015 and NHMS 2019 in this study. We assessed time and sociodemographic (age, sex, ethnicity and household income) trends in prevalence of adequate fruit and vegetables consumption between 2006 and 2019 among Malaysian adults.
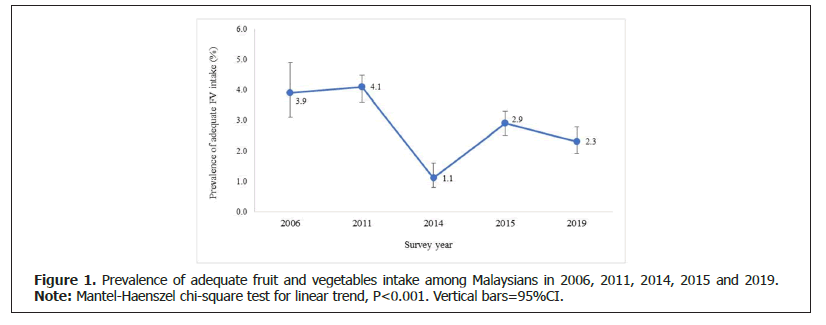
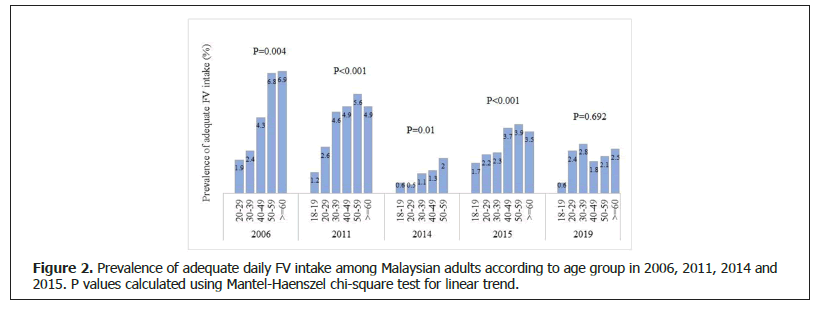
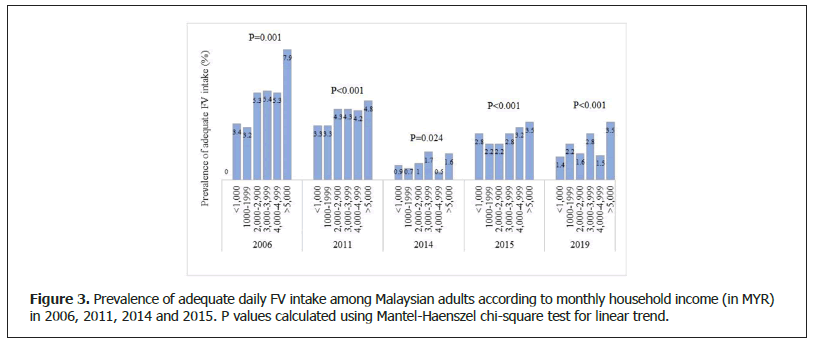
Results: We observed a significant downward trend in the prevalence of adequate fruit and vegetables consumption among the Malaysian adults between 2006 and 2019 with each successive survey (3.9%, 4.1%, 1.1%, 2.9% and 2.3%, respectively) (Ptrend<0.001). The prevalence of adequate fruit and vegetables consumption increased significantly with household income and age.
Conclusion: Our data showed a declining trend in fruit and vegetables consumption among Malaysian adults over the 13-year period, suggesting a need for a continuous effort to strengthen the existing healthy eating campaigns. This will not only increase the public awareness about the importance of adequate fruit and vegetables consumption to maintain an optimal health, but also aid in the effort to reverse the declining trend.
Keywords
Fruit and vegetables, Trend, Adults, Malaysia.
Abbreviations
FV: Fruit and Vegetables; NHMS: National Health and Morbidity Survey; NCDs: Non- Communicable Diseases.
Introduction
Fruits and vegetables are excellent sources of potassium, fibre, folate (folic acid), vitamin A, E, and C, as well as other minerals and vitamins. These nutrients are essential for good health, body function, and disease prevention [1]. Inadequate Fruit and Vegetables (FV) consumption is linked to increased risk of cardiovascular diseases, type 2 diabetes, certain types of cancers, obesity and all-cause mortality [2-7]. However, many Malaysian adults do not consume enough FV despite the well-known health benefits. The National Health and Morbidity Survey of 2019 reported a low percentage of Malaysians (5.1%) consumed enough fruits and/or vegetables [8].
The World Health Organization (WHO) recommends a minimum consumption of 400 grams or 5 servings of FV per day, however, countries may set their own recommendations for FV intake [9]. For instance, the 2020-2025 Dietary Guidelines for Americans recommend an intake of 1.5-2 cup-equivalents of fruits and 2-3 cup-equivalents of vegetables daily [10]. The Dietary Guidelines of Chinese Residents 2016 recommend a daily intake of 300-500 grams of vegetables and 200-350 grams of fruit (equivalent to 4-5 servings of FV), whereas the 2000 Dietary Guidelines for Japanese recommend 5-6 servings of vegetables and 2 servings of fruit and the Malaysian Dietary Guideline (MDG) 2010 recommended daily consumption of at least 5 servings of a variety of FV and (at least 3 servings of vegetables and 2 servings of fruit) for healthy adults [11-13].
In Malaysia, the consumption of adequate FV has been promoted in many health awareness campaigns. In MDG 2010, FV occupied the second tier of the Malaysian food pyramid. As a response to increases in diet-related, non-communicable diseases in Malaysia, the guidelines underwent a revision. In the new guidelines, MDG 2020, FV has swapped places with carbohydrates and is now positioned at the base of the pyramid, while the serving size of at least 5 servings per day recommendation has been maintained, further emphasize the importance of adequate daily intake of FV [13]. In addition to the revised MDG in 2017 the Malaysian Healthy Plate campaign was initiated, which aimed to emphasise the importance of increasing FV intake in a healthy diet. The Malaysian Healthy Plate promoted with the tagline Suku-Suku- Separuh (literal translation “Quarter-Quarter-Half”), illustrates the proportions of the food groups that should be consumed at each meal. The plate is divided into 3 portions, a quarter portion of grains, a quarter of protein (e.g., meat, fish, eggs), and the remaining half of the plate of FV [14]. Despite the various dietary campaigns conducted by government health agencies, data from several national surveys among Malaysian adults have shown low prevalence of adequate FV consumption [15-18]. In this study, we aimed to examine the trends in FV consumption among within large samples of Malaysian adults between 2006 and 2019. Our findings may assist the government in formulating better health policies aimed at promoting adequate FV intake in the Malaysian population.
Methodology
We analysed data from five nationally representative, population-based, health surveys, i.e. the Malaysian Non-Communicable Disease Surveillance 2006 (My- NCDS-1), the National Health and Morbidity Survey (NHMS) 2011, the NHMS 2014, NHMS 2015 and NHMS 2019 [8,15-18]. These five national surveys included assessments of Fruit and Vegetable (FV) intake among adults in Malaysia over the past two decades. We assessed the prevalence of adequate FV consumption and stratified by sociodemographic subgroups in each survey. The present study was approved by the Malaysian Ministry of Health Medical Research Ethics Committee (MREC).
Malaysian Non-Communicable Disease Surveillance 2006 (MyNCDS-1)
MyNCDS-1 was a cross-sectional, population-based survey, which was conducted between 2005 and 2006 to monitor the prevalence of NCD risk factors (diabetes mellitus, hypertension, dyslipidaemia, overweight/obesity, physical inactivity, smoking habits, alcohol intake and unhealthy dietary behaviours) in the Malaysian adult population. Two-stage stratified cluster random sampling was used to select a sample of Malaysian adults aged 25 to 64 years old. The total sample size was 2,572, all of which were included in this study [15].
National Health and Morbidity Survey 2011 (NHMS 2011)
NHMS 2011 was a population-based survey conducted between April and July 2011 aimed to provide community- based data on the prevalence of Non-Communicable Diseases (NCDs) such as diabetes, hypertension, hypercholesterolemia, and other health-related problems along with its risk factors in the Malaysian population. The target population was comprised of individuals residing in non-institutional living quarters [17]. Using a two-stage stratified random sampling method to select respondents, the target population was non-institutionalized residents of Malaysia with a total sample size of 28,498 respondents. However, only data from 18,191 adult respondents (aged above 18 years old) were included in this analysis.
National Health and Morbidity Survey 2014 (NHMS 2014)
The NHMS 2014 study was a population-based survey which assessed the eating habits, dietary intake, vitamins and minerals intake, food supplement usage, food security, nutritional status, and physical activity patterns among adults aged 18 to 59 years in Malaysia. Data collection for the survey took place between March and June 2014. A multi-stage stratified cluster sampling method was employed to select the respondents. This survey recruited a total of 3,000 respondents [16].
National Health and Morbidity Survey 2015 (NHMS 2015)
NHMS 2015 replicated the methodology and included most of the modules covered in the previous NHMS (NHMS 2011), but with a particular focus on healthcare demand and non-communicable diseases and their risk factors. A total of 29,490 respondents participated in this survey, but only data from 19,881 adult respondents were analysed [18].
National Health and Morbidity Survey 2019 (NHMS 2019)
The NHMS 2019 was the fourth NHMS with the similar methodology as the previous NMHSs. The risk factors of NCDs included physical inactivity, tobacco use, substance abuse, alcohol consumption, nutritional status, dietary practices, and health literacy. Additionally, health screenings were performed during the survey to detect breast, cervical, and colorectal cancers; erectile dysfunction; anaemia; children’s mental health issues; epilepsy; depression; and disability [8]. The NHMS 2019 was carried out between July and October 2019, which was a cross-sectional, population-based survey, that applied a multi-stage stratified cluster sampling technique. The survey recruited a total of 14,965 respondents. But for this study, only data from 8,428 adult respondents (age 18 and above) were extracted and analysed.
Sociodemographic information
All of the surveys collected sociodemographic data using interviewer-administered questionnaires. For this study, we extracted data on selected variables, which were comprised of residential areas (urban or rural), sex, age, ethnicity (Malay, Chinese, Indians, Other Bumiputra (Indigenous groups in Sabah and Sarawak), and household income. Age was categorised into 6 groups: 18-19 years, 20-29 years, 30-39 years, 40-49 years, 50-59 years, and ≥ 60 years. Monthly household income was divided into the following categories: less than MYR 1,000 (~USD 213), MYR 1,000-1,999 (~USD 213-426), MYR 2,000-2,999 (~USD 427-640), MYR 3,000-3,999 (~USD 641-853), MYR 4,000-4,999 (~USD 854-1067), and MYR 5,000 (~USD 1068) and above.
Fruit and vegetables intake measurements
Daily FV intake was assessed using four questions: 1) “In a typical week, how many days do you eat fruit?”; 2) “On the day that you usually eat fruit, how much did you eat?” or “How many servings of fruit do you eat on one of those days?”; 3) “In a typical week, on how many days do you eat vegetables?”; and 4) “On the day that you usually eat vegetables, how much did you eat on that day?” or “How many servings of vegetables do you eat on one of those days?”. Pictures of food serving sizes were used to aid participants in recalling the serving sizes of the fruits and vegetables consumed. These photographs depicted a single serving of commonly consumed fruits and vegetables. For example, one medium slice of papaya, watermelon, pineapple, or honeydew is considered a single serving of fruit. A cup of chopped raw leafy green vegetables, such as ‘ulam’ (local vegetables salad), or a half cup of cooked vegetables with edible stems (e.g., water spinach, choy sum, Chinese spinach), or a half cup of minced vegetables (e.g., carrot, ladyfingers, brinjal, tomato), is considered a single serving of vegetables. Adequate intake of vegetables was defined as ≥ 3 servings per day; adequate fruit intake was defined as ≥ 2 servings per day. Definition of adequate intake of FV according to MDG 2020, is ≥ 5 servings per day (i.e., at least 2 servings of fruit and at least 3 servings of vegetables) [13].
Statistical analysis
All statistical analyses were performed using SPSS software version 28 (IBM SPSS, Chicago). The analyses took account of unequal selection probability due to complex survey sampling. The sociodemographic characteristics of the respondents (i.e., residential area, sex, age groups and household income) were described in percentages with 95% confidence intervals (95% CI). The 95% CI were used to assess the significance of differences in the sociodemographic distribution of respondents between surveys. Pearson’s chi-square tests were performed to examine associations between sociodemographic factors and adequacy of FV consumption. The extended Mantel- Haenszel chi-square for linear trend was applied to investigate whether any linear trends were observed between age and household income and adequacy of FV intake. For all analyses, p values less than 0.05 were considered significant.
Results
The total number of participants in each survey was as follows: MyNCD-1 (n=2,572); NHMS 2011 (n=18,191); NHMS 2014 (n=2,993); NHMS 2015 (n=19,881); and NHMS 2019 (n=8,428). The prevalence of adequate FV consumption was 3.9%, 4.1%, 1.1%, 2.9% and 2.3% in MyNCD-1 2006, NHMS 2011, NHMS 2014, NHMS 2015, and NHMS 2019 respectively. In all the surveys, more than two-thirds of the respondents resided in rural areas. The gender distribution was approximately equal, the majority of respondents (approximately 50%) were between 20 and 39 years old and Malays (Table 1).
| Sociodemographic Characteristic | MyNCD-1 2006 (n=2,572) | NHMS 2011 (n=18,191) | NHMS 2014 (n=2,993) | NHMS 2015 (n=19,881) | NHMS 2019 (n=8,428) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated population | n | % (95% CI) | Estimated population | n | % (95% CI) | Estimated population | n | % (95% CI) | Estimated population | n | % (95% CI) | Estimated population | n | % (95% CI) | |||||
| Residential area | Rural | 40,99,400 | 1,277 | 34.2 (32.3, 36.1) | 1,30,05,590 | 7,607 | 73.2 (71.9, 74.4) | 1,35,87,391 | 1,408 | 69.3 (67.7, 70.9) | 1,53,48,505 | 8,407 | 76.2 (75.2, 77.2) | 1,27,84,597 | 5,143 | 79.1 (77.6, 80.6) | |||
| Urban | 78,99,400 | 1,295 | 65.8 (63.9, 67.7) | 47,70,869 | 10,584 | 26.8 (25.6, 28.1) | 60,13,035 | 1,585 | 30.7 (29.1, 32.3) | 47,91,917 | 11,474 | 23.8 (22.8, 24.8) | 33,71,569 | 3,285 | 20.9 (19.4, 22.4) | ||||
| Sex | Male | 62,17,599 | 1,044 | 51.8 (49.1, 54.6) | 90,70,451 | 8,512 | 51.0 (50.1, 51.9) | 1,02,26,855 | 1,384 | 52.2 (49.5, 54.8) | 1,03,96,458 | 9,455 | 51.6 (50.7, 52.5) | 78,97,201 | 3,739 | 48.9 (47.6, 50.2) | |||
| Female | 57,81,200 | 1,528 | 48.2 (45.4, 50.9) | 87,06,009 | 9,679 | 49.0 (48.1, 49.9) | 93,73,571 | 1,609 | 47.8 (45.2, 50.5) | 97,43,964 | 10,426 | 48.4 (47.5, 49.3) | 82,58,965 | 4,689 | 51.1 (49.8, 52.4) | ||||
| Ethnicity | Malay | 66,57,065 | 1,425 | 55.5 (52.4, 58.5) | 88,34,872 | 10,358 | 49.7 (46.9, 52.5) | 1,05,73,364 | 1,474 | 53.9 (49.5, 58.4) | 98,93,121 | 1,20,402 | 49.1 (46.4, 51.8) | 91,82,490 | 5,759 | 56.8 (52.5, 61.1) | |||
| Chinese | 20,49,144 | 461 | 17.1 (14.8, 19.6) | 45,29,338 | 3,521 | 25.5 (23.1, 28.0) | 37,99,064 | 516 | 19.4 (16.2, 23.0) | 47,18,263 | 3,173 | 23.4 (21.1, 26.0) | 39,22,732 | 1,147 | 24.3 (20.3, 28.7) | ||||
| Indian | 11,34,272 | 231 | 9.5 (7.7, 11.6) | 12,53,028 | 1,457 | 7.0 (5.9, 8.4) | 13,61,965 | 133 | 6.9 (5.3, 9.1) | 13,70,032 | 1,408 | 6.8 (5.9, 7.9) | 10,31,787 | 568 | 6.4 (5.1, 8.0) | ||||
| Non-malay bumiputra | 17,92,379 | 378 | 14.9 (13.4, 16.6) | 19,08,407 | 1,722 | 10.7 (9.2, 12.4) | 26,71,552 | 688 | 13.6 (12.0, 15.4) | 21,50,666 | 1,741 | 10.7 (9.3, 12.3) | 18,88,411 | 903 | 11.7 (9.7, 14.0) | ||||
| Others | 3,65,938 | 77 | 3.0 (2.2, 4.1) | 12,50,816 | 1,133 | 7.0 (5.8, 8.5) | 11,94,482 | 182 | 6.1 (4.8, 7.8) | 20,08,340 | 1,237 | 10.0 (8.4, 11.8) | 1,30,745 | 51 | 0.8 (0.4, 1.5) | ||||
| Age groups | 18-19 | NA | NA | NA | 8,87,222 | 782 | 5.0 (4.6, 5.5) | 11,14,241 | 130 | 5.7 (4.5, 7.1) | 9,47,242 | 798 | 4.7 (4.3, 5.2) | 6,02,798 | 235 | 3.7 (3.1, 4.4) | |||
| 20-29 | 19,82,109 | 269 | 16.5 (14.2, 19.2) | 53,05,493 | 4,197 | 29.8 (28.6, 31.2) | 53,68,392 | 688 | 27.4 (25.3, 29.6) | 56,16,288 | 4,086 | 27.9 (26.8, 29.0) | 40,64,349 | 1,443 | 25.2 (23.4, 27.0) | ||||
| 30-39 | 38,69,979 | 672 | 32.3 (29.5, 35.1) | 38,98,325 | 3,674 | 21.9 (20.9, 23.0) | 48,61,866 | 831 | 24.8 (22.8, 26.9) | 46,93,467 | 3,996 | 23.3 (22.3, 24.4) | 35,82,873 | 1,577 | 22.2 (20.4, 24.1) | ||||
| 40-49 | 33,53,413 | 797 | 27.9 (25.5, 30.6) | 32,83,490 | 3,634 | 18.5 (17.6, 19.4) | 46,02,902 | 755 | 23.5 (21.4, 25.7) | 35,19,617 | 3,651 | 17.5 (16.7, 18.3) | 27,54,738 | 1,441 | 17.1 (15.8, 18.4) | ||||
| 50-59 | 22,72,859 | 639 | 18.9 (16.9, 21.2) | 23,37,418 | 3,141 | 13.1 (12.4, 13.9) | 36,53,025 | 589 | 18.6 (16.9, 20.5) | 27,69,390 | 3,571 | 13.8 (13.1, 14.5) | 24,71,536 | 1,634 | 15.3 (14.2, 16.5) | ||||
| 60+ | 5,20,440 | 195 | 4.3 (3.6, 5.3) | 20,64,511 | 2,763 | 11.6 (10.8, 12.4) | NA | NA | NA | 25,94,418 | 3,779 | 12.9 (12.2, 13.6) | 26,79,872 | 2,098 | 16.6 (15.3, 18.0) | ||||
| Household income (RM), | <1,000 | 50,57,589 | 1,206 | 43.7 (40.7, 46.7) | 30,35,194 | 3,451 | 17.1 (15.9, 18.3) | 51,86,902 | 983 | 26.8 (24.3, 29.4) | 27,23,737 | 3,225 | 13.5 (12.6, 14.5) | 13,39,225 | 852 | 8.8 (7.7, 10.2) | |||
| 1000-1999 | 33,47,692 | 659 | 28.9 (26.1, 31.9) | 32,31,661 | 3,670 | 18.2 (17.0, 19.4) | 42,15,668 | 625 | 21.8 (19.6, 24.1) | 33,12,643 | 3,624 | 16.4 (15.4, 17.6) | 26,26,759 | 1,555 | 17.3 (15.5, 19.3) | ||||
| 2,000-2,999 | 16,51,123 | 301 | 14.3 (11.9, 16.9) | 29,91,811 | 3,084 | 16.8 (15.6, 18.1) | 31,08,667 | 450 | 16.0 (14.3, 18.0) | 32,60,634 | 3,362 | 16.2 (15.0, 17.4) | 25,08,218 | 1,360 | 16.5 (14.8, 18.5) | ||||
| 3,000-3,999 | 7,00,319 | 125 | 6.0 (4.6, 7.9) | 24,17,102 | 2,405 | 13.6 (12.5, 14.8) | 21,36,189 | 291 | 11.0 (9.5, 12.8) | 25,91,914 | 2,520 | 12.9 (11.9, 14.0) | 22,41,379 | 1,086 | 14.8 (13.1, 16.6) | ||||
| 4,000-4,999 | 3,98,159 | 82 | 3.4 (2.5, 4.7) | 18,52,012 | 1,660 | 10.4 (9.3, 11.6) | 12,10,733 | 167 | 6.3 (5.2, 7.5) | 19,82,176 | 1,788 | 9.8 (8.9, 10.8) | 15,22,742 | 756 | 10.0 (8.6, 11.7) | ||||
| >5000 | 4,28,397 | 98 | 3.7 (2.8, 4.9) | 42,48,680 | 3,921 | 23.9 (22.0, 25.9) | 35,11,385 | 448 | 18.1 (15.4, 21.2) | 62,69,319 | 5,362 | 31.1 (29.3, 33.0) | 49,25,041 | 2,284 | 32.5 (29.7, 35.4) | ||||
| Fruit and vegetables intake | Inadequate | 1,15,31,516 | 2451 | 96.1 (95.1, 96.9) | 1,70,55,524 | 17,464 | 95.9 (95.5, 96.4) | 1,93,85,675 | 2,949 | 98.9 (98.4, 99.2) | 1,95,64,597 | 19,281 | 97.1 (96.7, 97.5) | 3,68,364 | 164 | 97.7 (97.2, 98.1) | |||
| Adequate | 4,67,284 | 121 | 3.9 (3.1, 4.9) | 7,20,936 | 727 | 4.1 (3.6, 4.5) | 2,14,751 | 44 | 1.1 (0.8, 1.6) | 5,75,826 | 600 | 2.9 (2.5, 3.3) | 1,57,87,802 | 8,264 | 2.3 (1.9, 2.8) | ||||
Adequate FV intake varied across sociodemographic characteristics. The univariable analysis showed significant differences in the prevalence of adequate FV intake between urban and rural areas in two surveys, that is, NHMS 2011 and NHMS 2019. Specifically, urban residents had significantly higher FV intake than rural residents. Comparing adequate FV intake between genders, there was a significant difference in FV intake between men and women in NHMS 2015, wherein the prevalence of adequate FV intake was significantly higher among women than men. A significant association was observed between ethnic groups and adequacy of FV intake, in all the surveys except NHMS 2014 (Table 2). Linear trend analysis showed a significant downward trend in the prevalence of adequate FV consumption among Malaysian adults between 2006 and 2015 with each successive survey (Ptrend<0.001) (Figure 1).
| Sociodemographic Characteristics | MyNCD-1 2006 (n=2572) | NHMS 2011 (n=18,191) | NHMS 2014 (n=2,993) | NHMS 2015 (n=19,881) | NHMS 2019 (n=8,428) | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inadequate | Adequate | Inadequate | Adequate | Inadequate | Adequate | Inadequate | Adequate | Inadequate | Adequate | ||||||||||||||||||
| Overall (Ptrend<0.001) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |||||||
| 2451 | 96.1 (95.1, 96.9) | 121 | 3.9 (3.1, 4.9) | 17,464 | 95.9 (95.5, 96.4) | 727 | 4.1 (3.6, 4.5) | 2,949 | 98.9 (98.4, 99.2) | 44 | 1.1 (0.8, 1.6) | 19,281 | 97.1 (96.7, 97.5) | 600 | 2.9 (2.5, 3.3) | 164 | 97.7 (97.2, 98.1) | 8,264 | 2.3 (1.9, 2.8) | ||||||||
| Residential area | Rural | 1225 | 96.2 (94.7, 97.3) | 52 | 3.8 (2.7, 5.3) | 7,352 | 96.6 (96.0, 97.2) | 255 | 3.4 (2.8, 4.0) | 1,388 | 98.7 (97.9, 99.2) | 20 | 1.3 (0.8, 2.1) | 8,172 | 97.2 (96.5, 97.8) | 235 | 2.8 (2.2, 3.5) | 3234 | 98.2 (97.3, 98.8) | 51 | 1.8 (1.2, 2.7) | ||||||
| Urban | 1226 | 96.1 (94.7, 97.3) | 69 | 3.9 (2.9, 5.3) | 10,112 | 95.7 (95.1, 96.2) | 472 | 4.3 (3.8, 4.9) | 1,561 | 99.0 (98.4, 99.4) | 24 | 1.0 (0.6, 1.6) | 11,109 | 97.1 (96.6, 97.5) | 365 | 2.9 (2.5, 3.4) | 5030 | 97.6 (97.0, 98.1) | 113 | 2.4 (1.9, 3.0) | |||||||
| (p=0.132) | (p=0.025) | (p=0.433) | (p=0.790) | p=0.037 | |||||||||||||||||||||||
| Sex | Male | 994 | 96.3 (94.9, 97.3) | 50 | 3.7 (2.7, 5.1) | 8,187 | 96.2 (95.6, 96.7) | 325 | 3.8 (3.3, 4.4) | 1,367 | 99.1 (98.4, 99.4) | 17 | 0.9 (0.6, 1.6) | 9,227 | 97.6 (97.2, 98.0) | 228 | 2.4 (2.0, 2.8) | 3669 | 98.0 (97.3, 98.5) | 70 | 2.0 (1.5, 2.7) | ||||||
| Female | 1457 | 95.9 (94.5, 97.0) | 71 | 4.1 (3.0, 5.5) | 9,277 | 95.7 (95.0, 96.2) | 402 | 4.3 (3.8, 5.0) | 1,582 | 98.7 (98.0, 99.2) | 27 | 1.3 (0.8, 2.0) | 10,054 | 96.6 (96.1, 97.1) | 372 | 3.4 (2.9, 3.9) | 4595 | 97.5 (96.6, 98.1) | 94 | 2.5 (1.9, 3.4) | |||||||
| 2451 | (p=0.705) | (p=0.121) | (p=0.438) | p=0.001 | p=0.662 | ||||||||||||||||||||||
| Ethnicity | Malays | 1376 | 97.0 (95.6, 98.0) | 49 | 3.0 (2.0, 4.4) | 9,961 | 95.9 (95.3, 96.4) | 397 | 4.1 (3.6, 4.7) | 1,459 | 99.3 (98.6, 99.6) | 15 | 0.7 (0.4, 1.4) | 1,20,088 | 97.7 (97.2, 98.1) | 314 | 2.3 (1.9, 2.8) | 5669 | 98.1 (97.5, 98.5) | 90 | 1.9 (1.5, 2.5) | ||||||
| Chinese | 428 | 94.8 (92.1, 96.6) | 33 | 5.2 (3.4, 7.9) | 3,318 | 94.6 (93.4, 95.6) | 203 | 5.4 (4.4, 6.6) | 505 | 98.6 (97.2, 99.3) | 11 | 1.4 (0.7, 2.8) | 3,016 | 95.8 (94.6, 96.7) | 157 | 4.2 (3.3, 5.4) | 1106 | 96.7 (95.4, 97.6) | 41 | 3.3 (2.4, 4.6) | |||||||
| Indians | 222 | 97.5 (94.5, 98.9) | 9 | 2.5 (1.1, 5.5) | 1,425 | 98.3 (97.3, 98.8) | 32 | 1.7 (1.1, 2.7) | 131 | 98.9 (94.9, 99.7) | 2 | 1.1 (0.3, 5.1) | 1,367 | 96.8 (94.9, 98.0) | 41 | 3.2 (2.0, 5.1) | 556 | 97.7 (95.4, 98.9) | 12 | 2.3 (1.1, 4.6) | |||||||
| Other Bumiputras | 359 | 95.5 (92.6, 97.3) | 19 | 4.5 (2.7, 7.4) | 1,675 | 97.8 (96.9, 98.4) | 47 | 2.2 (1.6, 3.1) | 674 | 98.0 (96.4, 98.9) | 14 | 2.0 (1.1, 3.6) | 1,676 | 96.6 (95.3, 97.6) | 65 | 3.4 (2.4, 4.7) | 883 | 98.0 (96.3, 99.0) | 20 | 2.0 (1.0, 3.7) | |||||||
| Others | 66 | 84.7 (73.1, 91.9) | 11 | 15.3 (8.1, 26.9) | 1,085 | 96.1 (93.9, 97.5) | 48 | 3.9 (2.5, 6.1) | 180 | 98.7 (94.8, 99.7) | 2 | 1.3 (0.3, 5.2) | 1,214 | 98.4 (97.4, 99.0) | 23 | 1.6 (1.0, 2.6) | 50 | 99.9 (99.4, 100.0) | 1 | 0.1 (0, 0.6) | |||||||
| (p<0.001) | (p<0.001) | (p=0.276) | (p<0.001) | (p=0.031) | |||||||||||||||||||||||
| Age groups | 18-19 | NA | NA | NA | NA | 770 | 98.8 (97.9, 99.4) | 12 | 1.2 (0.6, 2.1) | 129 | 99.4 (96.1, 99.9) | 1 | 0.6 (0.1, 3.9) | 783 | 98.3 (96.9, 99.1) | 15 | 1.7 (0.9, 3.1) | 233 | 99.4 (97.0, 99.9) | 2 | 0.6 (0.1, 3.0) | ||||||
| 20-29 | 263 | 98.1 (95.6, 99.2) | 6 | 1.9 (0.8, 4.4) | 4,088 | 97.4 (96.7, 97.9) | 109 | 2.6 (2.1, 3.3) | 682 | 99.5 (98.8, 99.8) | 6 | 0.5 (0.2, 1.2) | 3,989 | 97.8 (97.2, 98.3) | 97 | 2.2 (1.7, 2.8) | 1412 | 97.6 (96.2, 98.5) | 31 | 2.4 (1.5, 3.8) | |||||||
| 30-39 | 650 | 97.6 (96.2, 98.5) | 22 | 2.4 (1.5, 3.8) | 3,523 | 95.4 (94.4, 96.2) | 151 | 4.6 (3.8, 5.6) | 820 | 98.9 (97.9, 99.5) | 11 | 1.1 (0.5, 2.1) | 3,887 | 97.7 (97.1, 98.2) | 109 | 2.3 (1.8, 2.9) | 1543 | 97.2 (95.8, 98.2) | 34 | 2.8 (1.8, 4.2) | |||||||
| 40-49 | 756 | 95.7 (93.9, 96.9) | 41 | 4.3 (3.1, 6.1) | 3,471 | 95.1 (93.9, 96.1) | 163 | 4.9 (3.9, 6.1) | 745 | 98.7 (97.2, 99.5) | 10 | 1.3 (0.5, 2.8) | 3,533 | 96.3 (95.3, 97.1) | 118 | 3.7 (2.9, 4.7) | 1420 | 98.2 (97.0, 98.9) | 21 | 1.8 (1.1, 3.0) | |||||||
| 50-59 | 595 | 93.2 (89.8, 95.6) | 44 | 6.8 (4.4, 10.2) | 2,979 | 94.4 (93.2, 95.4) | 162 | 5.6 (4.6, 6.8) | 573 | 98.0 (96.7, 98.9) | 16 | 2.0 (1.1, 3.3) | 3,434 | 96.1 (95.1, 96.9) | 137 | 3.9 (3.1, 4.9) | 1604 | 97.9 (96.6, 98.7) | 30 | 2.1 (1.3, 34) | |||||||
| 60+ | 187 | 93.1 (82.2, 97.5) | 8 | 6.9 (2.5, 17.8) | 2,633 | 95.1 (96.9, 96.1) | 130 | 4.9 (3.9, 6.1) | NA | NA | 3,655 | 96.5 (95.5, 97.3) | 124 | 3.5 (2.7, 4.5) | 2052 | 97.5 (96.3, 98.3) | 46 | 2.5 (1.7, 3.7) | |||||||||
| (Ptrend=0.004) | (Ptrend<0.001) | (Ptrend=0.01) | (Ptrend<0.001) | (Ptrend=0.692) | |||||||||||||||||||||||
| Household income (MYR) | <1,000 | 1160 | 96.6 (95.1, 97.7) | 46 | 3.4 (2.3, 4.9) | 3,333 | 96.7 (95.8, 97.4) | 118 | 3.3 (2.6, 4.2) | 973 | 99.1 (98.1, 99.6) | 10 | 0.9 (0.4, 1.9) | 3,131 | 97.2 (96.3, 97.9) | 94 | 2.8 (2.1, 3.7) | 1370 | 98.6 (97.6, 99.2) | 17 | 1.4 (0.8, 2.4) | ||||||
| 1000-1999 | 636 | 96.8 (94.3, 98.3) | 23 | 3.2 (1.7, 5.7) | 3,542 | 96.7 (95.9, 97.4) | 128 | 3.3 (2.6, 4.1) | 619 | 99.3 (98.3, 99.7) | 6 | 0.7 (0.3, 1.7) | 3,538 | 97.8 (96.9, 98.4) | 86 | 2.2 (1.6, 3.1) | 1530 | 97.8 (96.2, 98.7) | 25 | 2.2 (1.3, 3.8) | |||||||
| 2,000-2,999 | 280 | 94.7 (91.7, 96.6) | 21 | 5.3 (3.4, 8.3) | 2,970 | 95.7 (94.6, 96.6) | 114 | 4.3 (3.4, 5.4) | 443 | 99.0 (97.7, 99.5) | 7 | 1.0 (0.5, 2.3) | 3,271 | 97.8 (97.2, 98.3) | 91 | 2.2 (1.7, 2.8) | 1340 | 98.4 (97.3, 99.1) | 20 | 1.6 (0.9, 2.7) | |||||||
| 3,000-3,999 | 113 | 94.6 (89.9, 97.2) | 12 | 5.4 (2.8, 10.1) | 2,301 | 95.7 (94.6, 96.6) | 104 | 4.3 (3.3, 5.6) | 285 | 98.3 (95.0, 99.4) | 6 | 1.7 (0.6, 5.0) | 2,448 | 97.2 (96.2, 98.0) | 72 | 2.8 (2.0, 3.8) | 1058 | 97.2 (95.6, 98.3) | 28 | 2.8 (1.7, 4.4) | |||||||
| 4,000-4,999 | 75 | 94.7 (88.2, 97.7) | 7 | 5.3 (2.3, 11.8) | 1,595 | 95.8 (94.4, 96.9) | 65 | 4.2 (3.1, 5.6) | 165 | 99.5 (97.6, 99.9) | 2 | 0.5(0.1, 2.4) | 1,735 | 96.8 (95.5, 97.8) | 53 | 3.2 (2.2, 4.5) | 744 | 98.5 (97.1, 99.2) | 12 | 1.5 (0.8, 2.9) | |||||||
| >5,000 | 89 | 92.1 (82.1, 96.7) | 9 | 7.9 (3.3, 17.9) | 3,723 | 95.2 (94.1, 96.1) | 198 | 4.8 (3.9, 5.9) | 437 | 98.4 (96.9, 99.2) | 11 | 1.6 (0.8, 3.1) | 5,158 | 96.5 (95.6, 97.2) | 204 | 3.5 (2.8, 4.4) | 1699 | 96.5 (95.0, 97.6) | 53 | 3.5 (2.4, 5.0) | |||||||
| (Ptrend<0.001) | (Ptrend<0.001) | (Ptrend=0.024) | (Ptrend<0.001) | (Ptrend<0.001) | |||||||||||||||||||||||
The prevalence of adequate fruit and vegetables consumption significantly increased with age and household income in all of the surveys except NHMS 2019. A significantly higher proportion of those aged ≥ 60 years met the recommended FV intake compared to younger adults aged <30 years. Furthermore, a significantly higher proportion of adults with monthly household incomes MYR 5,000 and above had adequate FV intake than those with household incomes less than MYR 2,000 (Figure 2 and Figure 3).
Discussion
Our findings showed that the prevalence of adequate FV intake had not changed substantially from 2006 to 2019. In fact, there was a downward trend in FV consumption during these periods. Over 95% of Malaysian adults did not consume adequate FV. Similar observations have been reported by other Malaysian studies. An earlier study of 242 adults aged 18 and above in the state of Selangor reported an average consumption of FV of 173 grams per day, which was significantly lower than the recommended amount of 400 grams [19]. A more recent study by Ahmad et al., in a group of 279 young female students from a local public university revealed that approximately 87.8% of the respondents consumed fewer than 2 servings of fruits per day, while 93.6% consumed fewer than 3 servings of vegetables per day [20]. Another study by Eng and colleagues among 2,983 low-income adults residing in six low-cost flats in the Federal Territory of Kuala Lumpur also showed that 89.5% of the respondents did not meet the recommended daily intake of FV [21].
Regardless of the definition of adequate FV intake (whether ≥ 5 servings per day of FV, or 2 servings of fruit and 3 servings of vegetables) and the dietary assessment method used, the consumption of FV among Malaysian adults was still very low as compared to other countries. Two national surveys conducted in Thailand in 2004 and 2018 revealed that 26.6% and 34.4% of Thai adults aged >15 years, respectively, consumed at least 5 servings of FV daily [22,23]. According to the third wave of the European Health Interview Survey, approximately 12% of the population in the European Union (EU) consumed five or more portions of FV daily in 2019. Among the EU countries, the highest rates of daily intake of five portions or more of FV were in Ireland (33% of the population), the Netherlands (30%), Denmark (23%), and France (20%); while the lowest was in Romania, where only 2% of the population consumed at least five portions of FV. Bulgaria and Slovenia followed closely, Bulgaria reported 5%, and Austria reported 6% of prevalence of adequate FV intake [24]. There are several possible explanations as to why Malaysian adults consume insufficient FV. Health consciousness and knowledge about healthy eating have a significant positive effect on consumption of healthy food [25]. In other words, the low intake of daily FV could be attributed to inadequate knowledge surrounding the importance of consuming FV in achieving a balanced diet and improving overall health. A report from NHMS 2019 showed that about 83% of rural adults were unaware of the Malaysian Healthy Plate concept even after three years of its inception [14]. With rapid economic growth, coupled with urbanization and modernization over the past 30 years, Malaysian dietary habits have shifted to the consumption of more refined carbohydrates, high-fat foods, processed or convenience foods, and animal products, and this may have led to decreased intake of FV [26-28]. The cost of fresh FV can sometimes be higher than other food options, making them less affordable to the lower income group [21]. Putting all together, these pose more challenges to promoting greater FV consumption among Malaysian adults. Therefore, more efforts must be made to promote higher FV intake. This includes, modifying the food environment by increasing accessibility to healthier foods, including FV, in supermarkets, grocery stores and convenience stores, can influence health behaviours and promote healthier food choices. Such modifications may involve changing the store layout in order to make healthy foods more visually appealing, grouping healthier food items to showcase healthy options, and providing shelf labels with the nutritional value information of the healthier foodsn [29]. Promotion of FV intake should also be expanded to the electronic, print and social Medias through health talks or cooking demonstrations that emphasize the benefits of adequate FV intake in the prevention of NCD and nutrition-related health problems. There should also be a focus on improving understanding of food serving sizes, the food pyramid and the healthy eating plate [30].
This study demonstrated that FV consumption tended to increase with advancing age. Our finding mirrors the United States’ 2019 Behavioural Risk Factor Surveillance system report, which had a representative sample of 249,566 American adults aged ≥ 18 years in the United States as well as the 2011–12 National Nutrition and Physical Activity Survey of 2,337 young Australian aged 18–34 years [31,32]. However, other reports of FV intake in relation to age have shown otherwise. Two national surveys conducted in Thailand showed that the older age groups were more likely to consume insufficient amounts of fruits and vegetables compared to younger age groups. The Thailand National Health Examination Survey III which collected data from 39,290 individuals aged 15 years and above, reported that Thais aged ≥ 45 years had significantly lower intake of FV than those aged <30 years [23]. A similar study on a smaller scale, involving 6,991 participants from the four geographic regions of Thailand and Bangkok within the same age group, revealed that individuals aged ≥ 60 years were associated with insufficient FV intake compared to those aged 30-44 years [22]. However, a pooled analysis of data collected from 193,606 individuals aged ≥ 15 years in 28 low and medium-income countries between 2005 and 2016 revealed no association between FV consumption and age [33]. We offer the following explanations for the association between increasing age and FV consumption. Firstly, as people age, they tend to become more health-conscious and aware of the importance of a balanced diet. They may also seek to improve their overall health and well-being, leading to a greater consumption of nutritious foods like FV. Secondly, age-related health conditions and chronic ailments may motivate older individuals to learn about it, and adopt healthier eating habits, including higher FV intake. Furthermore, due to changing nutritional demands and health concerns, older persons may receive particular medical advice or recommendations from healthcare professionals to increase their FV intake [34]. Also as people age, with greater financial stability, they may settle in areas with better access to fresh produce, thus making it easier for them to incorporate FV into their diet, and also allowing them to afford a more diverse and nutritious diet, that includes an increased proportion of FV [35]. Besides, with the experience of being raised or exposed to rural/agricultural environments, in which FV is more, readily and cheaply, available, they may incorporate this concept into their diet and have more FV than the younger generation.
Our findings are consistent with the literature suggesting higher household income to be associated with increased consumption of FV. In a survey conducted among 1,200 adults who had visited shopping malls in seven cities in Malaysia, higher income was associated with more frequent purchase of FV and a tendency to spend more on FV in a week [36]. A study by Eng et al., also showed that low-income households tend to consume insufficient FV, and more than two-thirds of the respondents perceived FV as being moderately priced [21]. Low consumption of FV may be attributed to affordability concerns, as low-income households often prioritize purchasing meat products over FV due to their limited income [35]. This concurred with the US National Health and Nutrition Examination Survey (2015-2018) reported that the percentage of US adults aged 20 years and above who consumed any FV on a given day increased with family income levels [37]. Also, the Prospective Urban Rural Epidemiology (PURE) study, which assessed data related to FV consumption from 18 countries with different gross national income levels between 2003 and 2013, reported that per-person gross national income was positively associated with FV intake. Furthermore, the cost of one serving of vegetables or fruit relative to household income was more than 19 times higher in low-income countries than in high-income countries. The relative cost of one serving of fruit was 50 times higher in low-income countries than in high-income countries [38]. These factors are likely to explain the low consumption of FV among Malaysian adults with economic backgrounds. Therefore, to increase consumption of FV among those from low-income families, we advocate policies that support affordable access to FV. This can be done by providing financial assistance in the form of food vouchers to lower income families to purchase FV, besides encouraging community and urban farming initiatives [39,40]. Furthermore, authorities could engage with farmers to organize events such as farmers’ markets and provide incentives to support them in increasing their productivity and selling their products directly to consumers. These approaches aim to make FV more affordable, thereby promoting accessibility to a wider population [41].
Conclusion
In conclusion, our analysis of data spanning from 2006 to 2019 reveals a disconcerting decline in adequate fruit and vegetable consumption among Malaysian adults, despite dietary guidelines recommending daily servings. Adequate fruit and vegetable consumption was closely associated with higher household income and age; however, the overall consumption of fruits and vegetables among Malaysian adults remained unsatisfactory. The observed downward trend signals a critical public health challenge, given the well-established links between insufficient fruit and vegetable intake and various health risks. To address this issue, there is an urgent need for intensified and targeted interventions, encompassing robust public health campaigns, community engagement, and tailored strategies considering sociodemographic factors. Collaboration between government agencies, non-governmental organizations, and the private sector is crucial, supported by policy measures such as subsidies for fresh produce and incentives for healthier food retail practices. Continuous monitoring through national surveys is essential for assessing the effectiveness of interventions. By fostering a comprehensive and collaborative approach, Malaysia can strive to reverse this concerning trend, promoting a healthier population.
Limitations
Our study has several limitations. Firstly, FV intake was self-reported and thus susceptible to recall and social desirability biases, potentially leading to overestimation or underestimation of FV consumption across sociodemographic groups. Secondly, the data obtained from the national surveys involved non-institutionalized individuals only, thereby preventing the generalization of our findings to the entire adult population of Malaysia. Thirdly, all the surveys utilized a cross-sectional design, meaning that data was collected at a single point in time, thus limiting our ability to establish causal relationships. Despite these limitations, it is important to note that all the surveys employed a rigorous stratified multistage cluster probability sampling method. This approach ensured that the inclusion of a diverse range of participants representing different sociodemographic groups, resulting in a large and representative sample that allowed for the generalizability of the findings to the Malaysian adult population.
Acknowledgments
The authors would like to thank the Director General of Health Malaysia for his permission to publish this paper.
Author’s Contributions
KCC, TLK, and SMG were involved in the conceptualization and study design. KCC, TLK, SMG, LHL, and CYK performed data extraction, data analysis, and interpretation. KCC drafted the manuscript, and TLK, SMG, LHL, CYK, and MAO subsequently reviewed and edited the manuscript. All authors participated in manuscript revision and approved the final version.
Availability of data and materials
The data for this study are not publicly available, but they can be obtained upon reasonable request and with permission from the Director General of Health Malaysia.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the guidelines and regulations of the Institutional Review Board of the National Institutes of Health, Ministry of Health Malaysia. All the data extracted from the surveys, which was approved by the Malaysian Ministry of Health Medical Research Ethics Committee (MREC). The requirement for informed consent was waived by MREC because of the retrospective nature of the study.
References
- Slavin L, Lloyd B. Health benefits of fruits and vegetables. Adv Nutr. 2012; 3(4): 506-516.
[Crossref] [Google Scholar] [Indexed]
- Okuda N, Miura K, Okayama A, Okamura T, Abbott RD, Nishi N, et al. Fruit and vegetable intake and mortality from cardiovascular disease in Japan: A 24-year follow-up of the NIPPON DATA80 Study. Eur J Clin Nutr. 2015; 69(4): 482-488.
[Crossref] [Google Scholar] [Indexed]
- Wang PY, Fang JC, Gao ZH, Zhang C, Xie SY. Higher intake of fruits, vegetables or their fiber reduces the risk of type 2 diabetes: A meta-analysis. J Diabetes Investig. 2016; 7(1): 56–69.
[Crossref] [Google Scholar] [Indexed]
- Yip CSC, Chan W, Fielding R. The associations of fruit and vegetable intakes with burden of diseases: A systematic review of meta-analyses. J Acad Nutr Diet. 2019; 119(3): 464-481.
[Crossref] [Google Scholar] [Indexed]
- Nour M, Lutze SA, Grech A, Allman-Farinelli M. The relationship between vegetable intake and weight outcomes: A systematic review of cohort studies. Nutrients. 2018; 10(11):1626.
[Crossref] [Google Scholar] [Indexed]
- Wang DD, Li Y, Bhupathiraju SN, Rosner BA, Sun Q, Giovannucci EL, et al. Fruit and vegetable intake and mortality: Results from 2 prospective cohort studies of us men and women and a meta-analysis of 26 cohort studies. Circulation. 2021; 143(17): 1642–54.
[Crossref] [Google Scholar] [Indexed]
- Liu W, Hu B, Dehghan M, Mente A, Wang C, Yan R, et al. Fruit, vegetable, and legume intake and the risk of all-cause, cardiovascular, and cancer mortality: A prospective study. Clinical Nutrition. 2021; 40(6): 4316-4323.
[Crossref] [Google Scholar] [Indexed]
- Institute for Public Health (IPH). National Health and Morbidity Survey (NHMS) 2019: NCDs - Non-Communicable Diseases: Risk factors and other health problems. 2019.
- World Health Organization. Healthy diet. 2020.
- Harper AE. Dietary guidelines for Americans. Am J Clin Nutr. 1981; 34(1): 121–3.
[Crossref] [Google Scholar] [Indexed]
- Wang SS, Lay S, Yu HN, Shen SR. Dietary guidelines for chinese residents (2016): Comments and comparisons. J Zhejiang Univ Sci B. 2016; 17(9): 649-656.
[Crossref] [Google Scholar] [Indexed]
- Yoshiike N, Hayashi F, Takemi Y, Mizoguchi K, Seino F. A new food guide in Japan: The Japanese food guide spinning top. Nutr Rev. 2007; 65(4): 149–54.
[Crossref] [Google Scholar] [Indexed]
- National Coordinating Committee on Food and Nutrition (NCCFN). Malaysian Dietary Guidelines 2020. Ministry of Health Malaysia. 2021.
- Rahim NCA, Ahmad MH, Man CS, Zainuddin AA, Hasani WSR, Ganapathy SS, et al. Factors influencing the levels of awareness on malaysian healthy plate concept among rural adults in Malaysia. Int J Environ Res Public Health. 2022; 19(10): 6257.
[Crossref] [Google Scholar] [Indexed]
- Disease Control Division (NCD). Malaysia NCD Surveillance 2006 report. NCD risk factors in Malaysia. 2006.
- Institute for Public Health (IPH). National health and morbidity survey 2014 : Malaysian Adult Nutrition Survey (MANS) Vol. II : Survey findings. 2014.
- Institute for Public Health (IPH). National Health and Morbidity Survey 2011 (NHMS 2011). Vol. II: Non-Communicable Diseases. 2011.
- Institute for Public Health (IPH). National Health and Morbidity Survey 2015 (NHMS 2015). Vol. II: Non-Communicable Diseases, Risk Factors & Other Health Problems; 2015. 2015.
- Nurul IA, Aminah A, Pauzi MA, Lee YH, Wan RWM, Fatimah S. Patterns of fruits and vegetable consumption among adults of different ethnics in Selangor, Malaysia. Int Food Res J. 2012; 19(3): 1095–107.
- Ahmad Sirfan AS, Hamirudin AH, Sidek S. Assessment of fruit and vegetable consumption among female university students. Food Res. 2020; 4(5): 1451-1460.
[Crossref]
- Eng CW, Lim SC, Ngongo C, Sham ZH, Kataria I, Chandran A, et al. Dietary practices, food purchasing, and perceptions about healthy food availability and affordability: A cross-sectional study of low-income Malaysian adults. BMC Public Health. 2022; 22(1): 19.
[Crossref] [Google Scholar] [Indexed]
- Phulkerd S, Thapsuwan S, Thongcharoenchupong N, Soottipong GR, Chamratrithirong A. Sociodemographic differences affecting insufficient fruit and vegetable intake: A population-based household survey of Thai people. J Health Res. 2020; 34(5): 419-429.
- Satheannoppakao W, Aekplakorn W, Pradipasen M. Fruit and vegetable consumption and its recommended intake associated with sociodemographic factors: Thailand National Health Examination Survey III. Public Health Nutr. 2009; 12(11): 2192-2198.
[Crossref] [Google Scholar] [Indexed]
- Stea TH, Nordheim O, Bere E, Stornes P, Eikemo TA. Fruit and vegetable consumption in Europe according to gender, educational attainment and regional affiliation-A cross-sectional study in 21 European countries. PLoS One. 2020; 15(5): e0232521.
[Crossref] [Google Scholar] [Indexed]
- Al Mamun A, Hayat N, Zainol NRB. Healthy eating determinants: A study among malaysian young adults. Foods. 2020; 9(8): 974.
[Crossref] [Google Scholar] [Indexed]
- Tee ES. Nutrition of Malaysians: Where are we heading ? Malays J Nutr. 1999; 5(1): 87–109.
- Goh EV, Azam-Ali S, McCullough F, Roy MS. The nutrition transition in Malaysia; Key drivers and recommendations for improved health outcomes. BMC Nutr. 2020; 6: 1–14.
[Crossref] [Google Scholar] [Indexed]
- Noor MI. The nutrition and health transition in Malaysia. Public Health Nutr. 2002; 5(1): 191-195.
[Crossref] [Google Scholar] [Indexed]
- Anderson E, Wei R, Liu B, Plummer R, Kelahan H, Tamez M, et al. Improving healthy food choices in low-income settings in the united states using behavioral economic-based adaptations to choice architecture. Front Nutr. 2021; 8: 734991.
[Crossref] [Google Scholar] [Indexed]
- Tee ES. Development and promotion of Malaysian dietary guidelines. Asia Pac J Clin Nutr. 2011; 20: 455-461.
- Lee SH, Moore LV, Park S, Harris DM, Blanck HM. Adults meeting fruit and vegetable intake recommendations-United States, 2019. MMWR Morb Mortal Wkly Rep. 2022; 71(1): 1-9.
[Crossref] [Google Scholar] [Indexed]
- Nour M, Sui Z, Grech A, Rangan A, McGeechan K, Allman-Farinelli M. The fruit and vegetable intake of young Australian adults: A population perspective. Public Health Nutr. 2017; 20(14): 2499–2512.
[Crossref] [Google Scholar] [Indexed]
- Frank SM, Webster J, McKenzie B, Geldsetzer P, Manne-Goehler J, Andall-Brereton G, et al. Consumption of fruits and vegetables among individuals 15 years and older in 28 low- And middle-income countries. J Nutr. 2019; 149(7): 1252–1259.
[Crossref] [Google Scholar] [Indexed]
- Liu L, Qian X, Chen Z, He T. Health literacy and its effect on chronic disease prevention: Evidence from China’s data. BMC Public Health. 2020; 20(1): 1–14.
[Crossref] [Google Scholar] [Indexed]
- French SA, Tangney CC, Crane MM, Wang Y, Appelhans BM. Nutrition quality of food purchases varies by household income: The SHoPPER study. BMC Public Health. 2019; 19: 1–7.
- Othman KI, Karim MSA, Karim R, Adzhan NM, Halim NA. Consumption pattern on fruits and vegetables among adults: A case of Malaysia. Acad J Interdiscip Stud. 2013; 2(8): 424–430.
- Ansai N, Wambogo EA. Fruit and vegetable consumption among adults in the United States, 2015-2018. NCHS Data Brief. 2021; 397: 1–8.
[Crossref] [Google Scholar] [Indexed]
- Miller V, Yusuf S, Chow CK, Dehghan M, Corsi DJ, Lock K, et al. Availability, affordability, and consumption of fruits and vegetables in 18 countries across income levels: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet Glob Health. 2016; 4(10): e695–703.
[Crossref] [Google Scholar] [Indexed]
- Basu S, Akers M, Berkowitz SA, Josey K, Schillinger D, Seligman H. Comparison of fruit and vegetable intake among urban low-income us adults receiving a produce voucher in 2 cities. JAMA Netw Open. 2021; 4(3): e211757.
[Crossref] [Google Scholar] [Indexed]
- Hume C, Grieger JA, Kalamkarian A, D’Onise K, Smithers LG. Community gardens and their effects on diet, health, psychosocial and community outcomes: A systematic review. BMC Public Health. 2022; 22(1): 1247.
[Crossref] [Google Scholar] [Indexed]
- National Centers for Chronic Disease Prevention and Health Promotion. The CDC Guide to Strategies to Increase the Consumption of Fruits and Vegetables. Department of Health and Human Services. 2011.
Author Info
Kee CHEE CHEONG1*, Tan LAY KIM1, Sumarni MOHD GHAZALI2, Yong Kang CHEAH3, Lim HUI LI4 and Mohd Azahadi OMAR12Department of Biomedical Epidemiology, Institute for Medical Research, National Institutes of Health, Ministry of Health Malaysia, Shah Alam, Selangor, Malaysia
3School of Economics, Finance and Banking, College of Business, Universiti Utara Malaysia, Sintok, Kedah, Malaysia
4Clinical Research Centre, Hospital Sultan Ismail, Ministry of Health Malaysia, Johor Baru, Johor, Malaysia
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
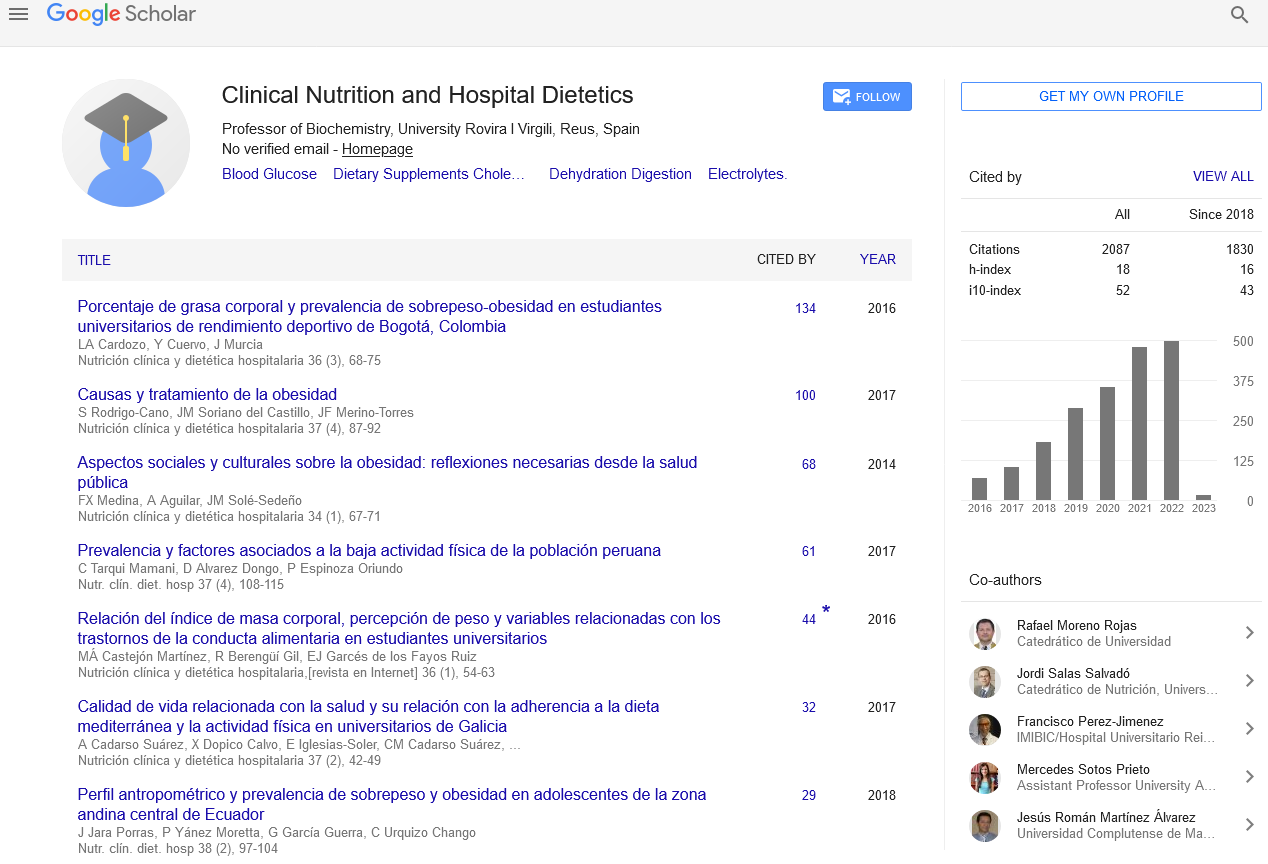
Google Scholar citation report
Citations : 2439
Clinical Nutrition and Hospital Dietetics received 2439 citations as per google scholar report
Indexed In
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- SCOPUS
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Web of Science
Journal Highlights
- Blood Glucose
- Dietary Supplements
- Cholesterol, Dehydration
- Digestion
- Electrolytes
- Clinical Nutrition Studies
- energy balance
- Diet quality
- Clinical Nutrition and Hospital Dietetics